Dr. Kindschuh news and updates:
- Dr. Gladstein gave tPA for a stroke in 24 minutes yesterday!
- Coney goal is <30 minutes
- Please clean your equipment (glidescopes, ultrasound, etc)
- 7a: Chirag / Denise – resident lectures (please send your topics to me soon – 20min max)
- 745a: Dan (rotating intern) – Syncope ED Pearls
- 8a: Dr Misch – Managing Unstable GI bleeds (non-administrative)
- 9a: Dr Viguri – Understanding Opioids
- 10a: Dr Patel – EKGs
- 11a: Dr Seeram – DKA/HHS — (not today)
- Pancreatitis – Chirag
- Pancreatitis dx, need ⅔
- 1) Epigastric tenderness
- 2) Lipase >3x normal
- 3) CT evidence
- Get triglyceride level
- Hypertriglyceridimic pancreatitis is treated with IV insulin (M-ICU admission)
- CT to look for complications, pseudocyst, necrotizing pancreatitis
- Get RUQ US
- Rule out gallstone pancreatitis
- Ranson criteria
- Mortality of panc on initial vs 48hr lab values
- BISAP: more specific than Ranson and APACHE II
- Treatment:
- LR > NS to prevent SIRS within first 24hrs
- Pain control: opioids but avoid if possible as per APA
- PO intake as tolerated
- Causes of acute pancreatitis: I GET SMASHED
- Pancreatitis dx, need ⅔
- Valvular Disorders – resident lecture – Faseeh
treated with diltiazem
- EKG with afib rate 140s, given Cardizem → new ekg shows NSR rate 75 (notched p-waves)
- LAE can cause compression of esophagus, causing cough/hoarseness
- CXR: showing enlarged LAE — loss of aortic knob:
- LAE on POCUS (parasternal long and apical 4 chamber view)
- Treatment in MR/MS in this pt
- Treat underlying rhythm
- If fluid overload: can use Dobutamine to increase inotropy; do not decrease preload
- Internet Book of critical care
- Think MI for MR or dissection for AR
- Acute symptomatic valve regurgitation requires EMERGENCY SURGICAL REPAIR OR REPLACEMENT
- Acute MR pts may benefit from an intra-aortic balloon pump if surgery is not immediately available
- Crashing afib patient, Dr. Rizzo:
- Unstable? Shock!
- Onset <24 hours, consider shocking in ED (more likely in Canada)
- Hypotensive? Start pressors (norepi, dobutamine)
- On CCB? Give calcium
- High dose mag help rate and rhythm control
- Afib lose 15% EF when in afib
- CHA₂DS₂-VASc Score for Atrial Fibrillation Stroke Risk
- Link Dr. Rizzo:
- Dan (rotating intern) – Syncope ED Pearls
- AliEM: Syncope as Easy as 1-2-3 Syncope as easy as 1-2-3
- Lateral tongue bites = seizure
- “Syncope AND ____”
- Syncope and abdominal pain: ruptured AAA
- Syncope and cancer, swollen leg, tachycardia: PE
- Syncope fever, cough, hypoxia: pneumonia
- Syncope and sudden onset HA: SAH
- Syncope and young woman + abdominal pain: Ectopic pregnancy
- Syncope and adolescent athlete: HOCM
- Abnormal “can’t miss” on ECG
- WPW
- Long/short QT
- HOCM
- Brugada
- ARVD (epsilon wave)
- Ischemic changes (t-waves, STEMI, Wellens, etc)
- Bundle branch blocks
- HOCM vs Brugada historical clue (Dr. Rizzo)
- HOCM occurs with exertion
- Brugada happens typically at rest
- Canadian Syncope Risk Score – externally validated
- San Francisco Syncope Rule (“CHESS”) – not externally validated
- PESI: Pulmonary Embolism Severity Index
- Let symptoms guide workup and treatment.
- Orthostatic vitals: are not diagnostic of syncope, not useful, not helpful, not indicated
- ALWAYS check for a MURMUR (Dr. Rizzo)
- If you hear MURMUR it is AORTIC STENOSIS until proven otherwise
- Dr Misch – Managing Unstable GI bleeds (non-administrative)
- Massive GI bleed management (first10EM)
- Massive definition: shock
- Admin stuff: use GBS and Rockall score
- Shock Class I will have normal vitals
- if unstable vitals → class II or III, be worried
- “Treat everyone as an upper GI bleed, don’t worry about melena vs bright red blood per rectum—upper GI patients die faster.” -Dr. Misch
- Most important test to send? (you only have one tube) = T&S
- NG tube discussion
- lavage sensitivity/specificity is poor
- Nasogastric aspiration and lavage in emergency department patients with hematochezia or melena without hematemesis (pubmed)
- Erythromycin infusion or gastric lavage for upper gastrointestinal bleeding: a multicenter randomized controlled trial (pubmed)
- Safe to place an NG tube with varices? YES (it’s safe)
- Per Eugene from GI attending: ‘varices don’t burst due to exterior manipulation, they burst due to increased pressure (portal HTN)’
- CTA for GI bleed diagnosis
- Rate of infusion by size of catheter
- 16G PIV is better than Cordis!
- Treatment
- BLOOD (1:1:1 Plasma:Platelets:RBCs)
- PROMMTT: The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) Study: Comparative Effectiveness of a Time-varying Treatment with Competing Risks
- PROPPR: Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial
- Goal directed transfusion: sbp 90-100; hgb 7
- Pt have better outcomes with strategic transfusion
- Hgb goal? Hgb 7 generally, Hgb 9 if CAD
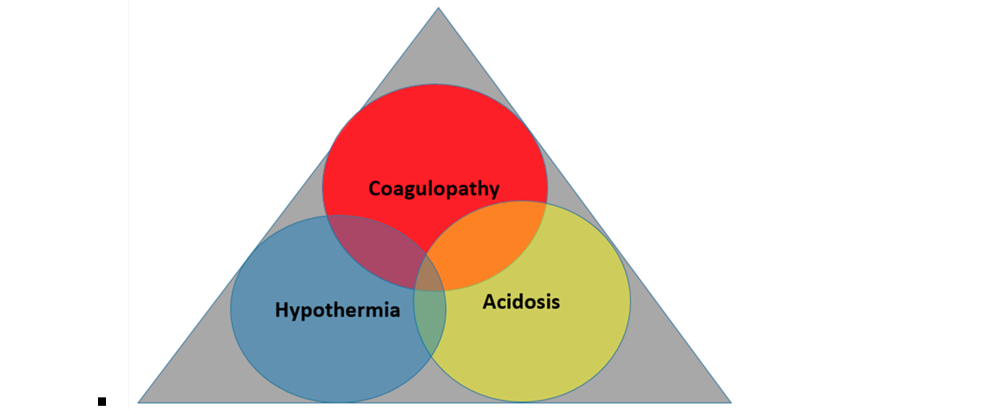
- Lethal triad:
- Reverse anticoagulation
- FFP
- Andexanet alpha – sucks, $$$
- PCC
- TXA (no benefit)
- PPI: no improvement in mortality (Cochrane)
- May have a slight decreased hemorrhage if they are to scope the next day.
- Proton pump inhibitor treatment initiated prior to endoscopic diagnosis in upper gastrointestinal bleeding
- Intubation
- HUGE ASPIRATION RISK!
- NGT (to stop blood aspiration)
- Consider seated intubation/tomahawk if you have done before.
- Consider gastric diversion during intubation, intubate the esophagus!
- Use Decanto suction catheter vs yankauer
- HOP patients (original podcast: How to Safely Intubate the Shocked Patient) but weingart has many more…
- Hypotension
- Oxygenation
- PH and ventilation
- Consider Tomahawk intubation
- Unstable for endoscopy?
- Blakemore tube for tamponade
- Liver failure and esophageal varices
- Octreotide: trend towards decreasing blood product need, no mortality benefit
- Antibiotics: Ceftrixaone, only medicine with mortality benefit
- These pts have high INRs–do not need to correct, it will just be excess volume → increase circulation in portal venous system → more bleeding
- TIPS (at some later date)
- Take home points:
- Massive GI bleed
- NGT is safe
- Intubation is very difficult and dangerous
- Consider Tomahawk intubation + Gastric diversion
- Decanto > Yankauer (set up 2)
- Access is KING
- need 2 or more lines, as large gauge as possible.
- Do the things that will SAVE their life, focus on the things that matter:
- Reverse anticoagulants
- Antibiotics
- Massive GI bleed
- HUGE ASPIRATION RISK!
- Dr Viguri – Understanding Opioids “What you should know when prescribing and available alternative”
- MME = morphine milligram equivalents
- ED Prescribing laws for opioids in NY
- 7 day prescribing limit
- NJ law: must prescribe naloxone if prescribing >90 MME, or if opioid + benzo simultaneously
- MME/day = dosage x doses per day x MME conversion factor
- Dosages >50 MME/day x2 risk for OD
- Alternatives:
- NSAID, tylenol (975mg pain dose), topical (lidocaine, diclofenac), gabapentin, muscle relaxants, droperidol, ketamine (can cause increased myocardial demand: tachycardia +HTN)
- Trigger point injections
- PT, OMT, acupuncture, low dose antidepressants, CBT, pain management referral
- Migraine treatment
- 1) Toradol, tylenol, reglan/zofran/compazine, IVF
- 2) Mag, haldol, sumatriptan, ketamine
- Droperidol > compazine
- ED headache algorithm: ED Management of Headache Algorithm
- Hyperemesis cannabinoid:
- (0.075%) Capsaicin can relieve discomfort (case studies)
- 1100a: Dr Patel – EKGs
- 69M hx of MG, hypothyroid, bipolar (on lithium) with generalized weakness, hypotension 60/40, brady 40s on arrival
- EKG
- 1st ECG: 1st degree AV block, bradycardia, RBBB, Q wave in III and aVF, hyperacute T wave aVF
- CXR no PTx
- Labs Cr. 2.9, Trop 0.9
- 2nd ECG: Anterior ST depressions (concern for posterior MI), 2nd degree type 1 mobitz block: Wenckebach (No acute treatment for this block)
- Becomes agitated, given 1 ativan → patient codes → ROSC
- 3rd EKG: 3rd degree AV block, complete dissociation of p-waves and QRS complexes
- V2-v4 depression, next step?
- Get POSTERIOR EKG, may be POSTERIOR MI
- DeWinters = STEMI equivalent
- STD with hyperacute T-wave
- 4th ECG: accelerated idioventricular
- Evolution of a STEMI:
- Lithium toxicity
- Processed renal, AKI → lithium toxicity
- Lithium toxicity = indication for STAT DIALYSIS
- Myasthenia crisis
- Severe weakness? Intubate and MICU
- Mild? Pyridostigmine
- Steroids make it worse, useless in acute setting; take weeks for to take effect
- Plasmapheresis: we can’t do at Coney, someone has to come in to do it from the city; we use IVIG
- 1130a: Dr Patel – Clinical EKGs
- A fib RVR 160s (hypertensive)
- Tx:
- Cardizem (1st dose: 0.25mg/kg, 2nd dose 0.35mg/kg + chase with PO)
- Metoprolol
- High-dose Magnesium (4g)
- Digoxin
- Amiodarone
- Procainamide
- Shock
- Metoprolol and cardizem: AV node blockers
- (Case reports of using BOTH cardizem and metoprolol can → complete AV block)
- Tx:
- A fib RVR 160s (relative hypotension 90/60)
- Still treat with cardizem→ heart may need to slow down to return blood flow to heart and increase bp
- A fib RVR 160s (severe hypotension 70/30)
- Dig, amio, push dose epi, fluids, shock
- Rate related stuff (Dr. Rizzo)
- Rate related STD DOES exist
- Rate related troponin rise DOES NOT exist
- If you increase Troponin from SVT = failed stress test
- PROGNOSTIC UTILITY OF CARDIAC TROPONIN ELEVATION IN PATIENTS PRESENTING WITH SUPRAVENTRICULAR TACHYCARDIA
- Atrial flutter
- Usual rate: 300-150-100
- SVT
- Can use cardizem/metoprolol especially if you aren’t sure if SVT vs Aflutter.
- Adenosine
- Vagal maneuvers
- Pericarditis vs STEMI (Amal Mattu)
- STEMI VS. ACUTE PERICARDITIS – ECG Weekly
- Differentiating STEMI from Pericarditis — JournalFeed
- Look for signs to rule in STEMI on ECGs with ST elevation in the following steps before looking for any ECG changes associated with pericarditis:
- 1) Search for ST depression (aside from leads aVR and V1)
- 2) Look for ST elevation in lead III > II
- 3) Search for horizontal or convex upward ST elevation
- T-wave inversions ddx
- Ischemia
- Brain bleed
- PE (anterior-inferior)
- HOCM w strain
- LVH w strain
- A fib RVR 160s (hypertensive)
- 11a: Dr Seeram – DKA/HHS
- Moved to other date