Mini Case Report
HPI
68 yo F with PMHx of Polio, HTN and arrhythmias presents to the ED with abdominal pain and nausea X 1 week. Pain is in the periumbilical region,10/10 intensity, squeezing in nature, radiates to the epigastric region and is not responsive to OTC pain meds and omeprazole. She also endorsed chills, shortness of breath, diarrhea that started the day prior. She denies fever, chest pain, palpitations, vomiting, headache, LOC, constipation. Pt still has her appendix, PSHx of Gastric bypass 12 years prior.
PE
Moderate epigastric and mild periumbilical tenderness to palpation. Remainder of the exam is unremarkable.
Initial Tx
Pt given Toradol, Pepcid and Zofran, symptoms resolved
Workup (abnormal labs)
EKG: NSR with prolonged QTc
Hypokalemia: 3.0
Mild leukocytosis: CBC 13.25
Additional Tx
Potassium and Magnesium repleted.
Pt signed out to the oncoming team and on reassessment nausea and pain has returned. Physical exam significant for TTP in RLQ, no epigastric or rebound tenderness. Pt is given a second dose of Zofran and Toradol for symptomatic relief. Appendix ultrasound showed no appendicitis. While waiting for CTAP results pt starts to have sharp pain in different abdominal locations, no relief with change in position.
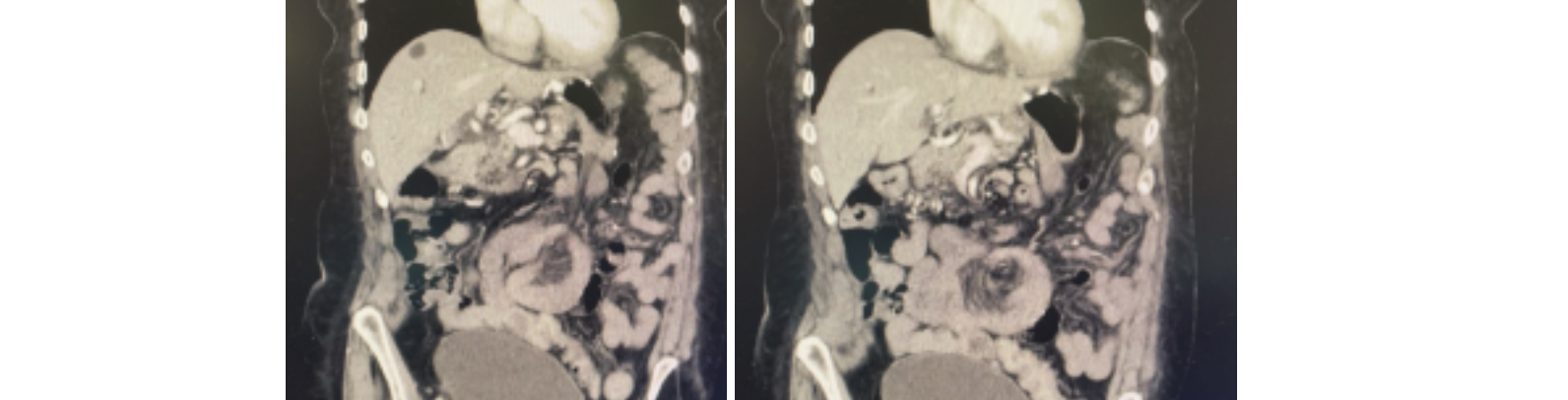
CTAP images & read:



There is swirling of multiple small bowel loops in the mid abdomen with associated mesenteric fluid and fat stranding. There is prominence of and swirling of the mesenteric vessels. Findings are highly suspicious for internal hernia.
Pt is taken to OR or emergent laparotomy.
Brief Surgery Findings:
internal hernia with twisted bowel and mesentery, long segment of threatened bowel, with frankly ischemic segment of roux limb which was forming a band around the twist. Roux limb transected to release hernia/volvulus with immediate resolution of color of threatened bowel, segment of roux limb remained ischemic. Ischemic segment of roux limb resected from gastric remnant to just distal viable roux limb, and gastrojejunostomy performed. Anastomosis buttressed with omentum, leak test performed after passing NGT past anastomosis. 10F JP drain placed.
Discussion
So, what exactly is an internal hernia? Essentially it’s when your bowels get tangled up like a box of old Christmas lights. It’s a SBO that occurs from a closed loop. Medically defined as “protrusion of abdominal viscera, most commonly small bowel loops, through a peritoneal or mesenteric aperture into a compartment in the abdominal and pelvic cavity” (1). Based on the variation of anatomy this may happen in a variety of ways. Bowels can herniate through normal anatomy (like the foramen of winslow) or may be provoked from inflammation, trauma, liver transplant, and gastric surgery. The Pt’s history of a Gastric bypass surgery is an important aspect to suspect obstructive pathologies. The incident of a transmesenteric internal hernia is more common after Roux-en-Y loop surgery and is shown in the image below:

Diagnosis is best made with a CT scan. Twisting of the bowel around a central area, known as a “mesenteric swirl” sign has been the most predictive sign of internal hernia (sensitivity 78-100%, specificity 80-90%) (2). Other specific CT findings may be clusters of bowel loops (see above). Internal hernias account for 5.8% of SBO with a mortality rate over 50% (3). ��
References:
1. Miller PA, Mezwa DG, Feczko PJ, Jafri ZH, Madrazo BL. Imaging of abdominal hernias. Radiographics. 1995;15:333–47
2.Iannuccilli JD, Grand D, Murphy BL, Evangelista P, Roye GD, Mayo-Smith WSO Clin Radiol. 2009;64(4):373. Epub 2008 Dec 16.
3. Kar S, Mohapatra V, Rath PK. A Rare Type of Primary Internal Hernia Causing Small Intestinal Obstruction. Case Rep Surg. 2016;2016:3540794.