- 7a: Resident Lectures: Eugene – Steroids / Hamzah – Non-traumatic vision loss (both really cool topics)
- 8a: Dr Sun – Hyperkalemia / Mike Cyd – CCU/EKG lecture #1
- 9a: BREAK / TJ – SIM LAB
- 10a: TJ – SIM LAB
- 11a: TJ – SIM LAB
- QA with Dr. Kindscuh
- Talked about some recent cases with potential lawsuits
- Methadone OD should get ICU consult and at the very least admitted for tele for 24 hours
- GI code
- Rockall score >10% → go to resus room
- GBS score >50% → get GI fellow down
- We will be switching from alteplase to tenecteplase
- SEPSIS code, call them more often, we need more data
- Don’t use oral contrast for CTAP unless it is indicated
- Appy with BMI <20
- Low grade SBO (c/i in high grade → nausea/vomiting/aspiration)
- Intraabdominal abscess
- New interpreter devices for cyracom are available
- Breezy point event August 11 (dress code business casual)
- Hamzah – Non-traumatic vision loss
- All patients require: Visual Acuity, Pupils, Confrontational Visual Fields, EOM, IOP, CN exam, POCUS (NOT in globe rupture)
- Hamzah’s case: Pt with Central Retinal Art Occlusion
- Painless: Retinal Detachment, CRAP, CRVO, Giant Cell Arteritis
- GCA
- (must have 3 of 5 to diagnose): >50yo, temporal artery tender, ESR >50, headaches, (+biopsy)
- Tx: ROIDS (Methylprednisolone 1000mg QID x3 days)
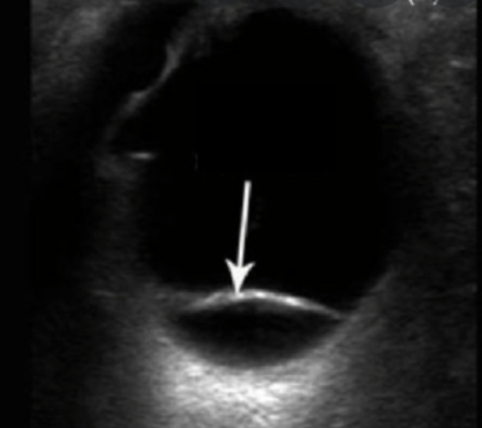
- Retina detachment
- Sudden painless, flashes/floaters, “curtain”
- TJ tidbit: If macula on, then vision can be saved if surgery within 24hrs
- POCUS is Dx test of choice in ED
- CRAO
- “Cherry red macula”
- CRVO
- “Blood and thunder”
- CRAO vs CRVO
- GCA
- Painful: Glaucoma, Uveitis, Optic neuritis
- Acute Angle Closure Glaucoma
- Hazy Cornea, fixed irreg pupil
- IOP >40
- MEDS: Timolol (BB), Pilocarpine (causes meiosis)
- POCUS: 3×5 rule for ICP elevation, may be extrapolated to IOP(?)
- Iritis or Anterior Uveitis (not just bilateral conjunctivitis)
- Ciliary flush
- Pain >> normal
- Management: Cycloplegics (atropine), steroids, Ophtho f/u in 24 hours
- Acute Angle Closure Glaucoma
- Eugene – Steroids
- Sepsis case, IVF + pressors not working… Next step? Steroids
- Steroid Effects:
- Point/Counterpoint from PulmCrit on Steroids in Septic Shock
- Comparison of APPROCCHSS vs ADRENAL trials
- https://emcrit.org/pulmcrit/aprocchss/
- Hydrocortisone
- 5 half lifes for any drug to be eliminated
- Steroids Indicated in bacterial meningitis → SPECIFICALLY Dexamethasone
- 2-3 weeks of hydrocortisone to get adrenal suppression from steroid use
- Solumedrol vs Hydrocortisone? Hydrocortisone has both mineralocorticoid and glucocorticoid activity
- Dr Sun – Hyperkalemia
- Mike Cyd – CCU/EKG lecture #1
- Bradycardic patient, HR 30s, BP 140/80
- DDx for bradycardia: HE DIE “hypothermia, endocrine, drugs, ischemia, electrolytes”
- BB vs CCB toxicity?
- BB = hypoglycemia
- CCB = hyperglycemia
- TJ – SIM LAB
- ATLS SIM
- 57M fell off a 7 foot ladder, unwitnessed
- ABCDE
- Hypotensive/bradycardic = neurogenic shock
- Neurogenic shock
- 1st line pressor = norepi
- MAP target = 85 (not 65 like sepsis)
- If worries about neck trauma and pt is in a c-collar intubate with glide.
- Oral boards cases with Geoff
- Case 1
- 72M ICD constantly shocking patient, EKG shows WCT consistent with Vtach, treated with procainamide or amiodarone
- Case 2
- 34M palpitation and lightheadedness after cocaine use, EKG showed SVT, treated with adenosine, had a seizure which resolved with Ativan, then Vtach (WCT)
- Cocaine toxicity wide complex tachycardia is treated with 2-4 amps sodium bicarbonate (against ACLS protocol)
- Amio may work but procaína mide will increase sodium channel blockade and cause torsades as cocaine is a sodium channel blocker
- Case 1