Residency/Department Updates
- Next week’s 10/20 conference will be over Zoom
- 10/27 conference will be a reverse conference day
- Princess shift 7am-1pm
- Conference will be in person around the Coney Island board, full schedule will be e-emailed soon.
- 7a: Dr Jeong / Dr Rizzo / Peds EM faculty: CCA GI Bleed
- 830a: Peds EM faculty: CCA GI Bleed
- 930a: Resident Lectures: Ivan / Jessica
- 1030a: Faseeh – EKG/CCU #3 / Jessica – Toxicology Lecture (or Ultrasound)
- 1130a: Kaiser Permanente Physician – Job Searches and CV writing w/ Q+A (There will be food)
Resources for GI Bleed ‘Core Clinical Application’ discussion:
EMRAP C3
- C3 – Massive GI Bleed
- C3 – Minor/Stable GI Bleeding
- PDF Summaries
EMCases
EMCrit
Dr Jeong / Dr Rizzo / Peds EM faculty: CCA GI Bleed
- Identification
- Upper GI
- Hematemesis
- GI: “coffee ground emesis is not an emergency”
- Hematemesis
- Lower GI
- BRBPR + clots
- Upper GI
- Risk stratification
- Case 1
- 84F HTN DM, normals vitals, “looks good”
- Rockall score = 4 = 24% mortality prior to endoscopy
- Rockall score >3 → straight to RESUS ROOM
- Rockall score (MDCalc)
- VALIDATED – Validation of the Rockall scoring system for outcomes from non-variceal upper gastrointestinal bleeding in a Canadian setting
- age/shock/comorbidities
- Glasgow-Blatchford Score (MDCalc)
- Do not use to dc low risk patients, use to escalate care
- labs/clinical sx/medical history/vitals
- >6 is about 50% need intervention
- Sick or not sick
- “They look pretty good.”
- Be quicker to Upgrade patients and downgrade them later
- Case 1
- Workup
- Rectal exam
- Fecal occult?
- GI: “we don’t care about FOBT, don’t do it”
- Low sensitivity (24.3%), low specificity
- Intended for Colon Cancer screening, not detecting GI bleeding
- FOBT false positives: Colchicine, iodine, boric acid, red meat
- FOBT false negatives: Vitamin C
- It’s Time to Abandon Fecal Occult Blood Testing in the Emergency Department (ACEPnow)
- Labs
- T&S, CBC, BMP, Hepatic function panel, Coags
- BUN– higher levels more suggestive of upper GI bleed
- Predictors of upper GI bleed:
- Melena
- BUN:creatinine ratio >30
- Age < 50 years
- Coffee-ground emesis
- Coffee Grounds Emesis: Not Just an Upper GI Bleed (JofEM)
- Can be causes by multiple etiologies, not just GI
- “Conclusion: Although patients were admitted for UGI bleeding, the more significant associated diagnoses included acute myocardial infarction, urosepsis, small bowel obstruction, bilateral pulmonary emboli, and acute renal failure. Hemodynamically stable patients presenting with coffee grounds NG aspirate and no fall in hemoglobin/hematocrit should be evaluated for other non-GI bleeding-related conditions even as the GI bleed is being managed.”
- Rectal exam
- Management/Disposition
- Mild
- IVF, (consider Pepcid/Protonix depending on etiology)
- Dispo: likely discharge
- Moderate
- Dispo: more variable
- Severe
- First priority: IV access + blood
- Patients crash quickly, be ready for everything
- Airway (2 suctions, direct/glide/bougie)
- can MacGyver 10 ETTs to suctions
- Yankauer VS. Size 10 ETT
- SALAD intubation
- Essential Elements of SALAD by James DuCanto MD
- Resuscitation of the Hemorrhagic Shock Patient in Trauma
- RSI meds: less sedative, more paralytic
- ‘Any sedative agent you give is going to SHARPLY reduce the patient’s catecholamine response–which is the only thing keeping them alive RIGHT NOW.’
- ‘USE HIGHER doses of paralytic:, it is going to take some time to work the patient is vasoconstricted likely and not well perfusing. Use double dose rocuronium.’
- May need push dose pressors or infusion
- Monitor
- Two 16G IVs
- Airway (2 suctions, direct/glide/bougie)
- Closed-loop communication -important
- Consider NG tube, Blakemore tube
- Reverse anticoagulation
- Anticoagulant reversal (EMCrit)
- Monitor fibrinogen – for cryoprecipitate, Fibrinogen, factors 8,13, vWF
- TEG: Thromboelastogram (TEG) • LITFL • CCC Investigations
- TXA – not shown to be effective
- Calcium (RBCs → hypocalcemia)
- “Diamond of death”
- Priority of medications
- Ceftriaxone (if cirrhosis)
- Reduces mortality
- NNT 22 to prevent death
- NNT 4 to prevent infection
- Octreotide (all UGIB patients)
- Erythromycin (30min prior to endoscopy for suspected peptic ulcer)
- NNT 10 to decrease need for endoscopy
- Metoclopramide is an alternative (prokinetic)
- Pantaprazole 80 mg IV bolus (no infusion necessary)
- Decrease need for repeat endoscopy
- Proton pump inhibitor treatment initiated prior to endoscopic diagnosis in upper gastrointestinal bleeding (Cochrane review)
- Ceftriaxone (if cirrhosis)
- Interventional radiology
- If bleeding on CT angio
- General surgery
- Last resort
- Dispo: MICU
- Mild
- Some additional links:
- Massive GI bleed management (First10EM)
- LVAD Management in GI Bleed | CritCases (EMCases)
Peds EM faculty: CCA GI Bleed
- 15% of circulating blood volume may be lost prior to changes in vital signs
Upper GI Bleed
- Case 1—NOT SICK
- ROS: rash, weight loss, FTT, wet diapers
- Meds: ASA, phenytoin, phenobarb, abx, iron
- Trauma
- BH: Location of birth, cephalohematoma, etc.
- Case 2–-SICK
- Neonatal Upper GI Bleed
- Swallowed maternal blood
- Allow feeding in the ED
- Apt test: put blood in alkaline solution, neonatal blood will remain bright red (mom’s goes brown – denature)
- Hx of painful nursing
- Gastritis / Peptic Ulcer
- Prolonged hospital / NICU stay
- Vitamin K deficiency
- Parents refused or home delivery
- Swallowed maternal blood
- Infancy Upper GI Bleed
- Gastritis
- Mallory-Weiss tears
- School age/adolescence upper GI
- Epistaxis
- Esophageal/gastric varices (2/2 portal vein thrombosis 2/2 umbilical catheterization)
- Mallory weiss
- PUD
- Foreign body
- Caustic ingestion
Lower GI Bleed
- Case 3–-SICK
- Imaging: abdominal x-ray
- Pneumatosis intestinalis–air and gas in bowel wall
- Case 4–Not sick–passed polyp
- Neonatal Lower GI Bleed
- Necrotizing enterocolitis (NEC)
- Premature (Birth complications eg maternal cocaine use, IUGR, heart complications etc), feeding intolerance, abdominal distension
- Hirschsprung
- Delayed passage of meconium
- Consider partial Hirschcprungs
- Hirschsprung enterocolitis3 (kinda like toxic megacolon) – can be fatal, can happen years after repair
- Necrotizing enterocolitis (NEC)
- Infancy Lower GI Bleed
- Anal fissure–MOST COMMON CAUSE of lower gi bleeding in first 2 years of age (rosh question)
- Can cause chronic fissures (skin tags, chronic constipation, GI f/u)
- Bloody, not mucoid
- Polyps
- Painless rectal bleeding
- Juvenile polyps, > 5 through GI, 10-15% malignancy chance, f/u w/ GI
- Intussusception
- Telescoping of intestine
- Sausage mass in RUQ/”Currant Jelly” stools (late finding), both actually in <15% of patients
- Tx: Air enema
- Meckel’s diverticulum
- Remnant of vitelline duct
- Gastric mucosa or pancreatic tissue
- 2% of population, usually 2 types of tissues, 2 inches from ileocecal junction, 2 year olds
- Colitis
- Infectious, cows milk protein allergy, FPIES (food protein-induced enterocolitis-SEVERE)
- Hypovolemic shock + colitis = FPIES
- Anal fissure–MOST COMMON CAUSE of lower gi bleeding in first 2 years of age (rosh question)
- School age/adolescent LOWER GI Bleed
- Polyps
- IBD
- HUS
- HSP
- Angiodysplasia – rare, usually small bowel, massive hemorrhage
- Vascular lesions
- MANAGEMENT
- Guaiac?
- Lots of false positive/negatives, not sensitive/specific
- NG lavage
- Imaging
- Antibiotics?
- Salmonella?
- If <3months of age TREAT; or if septic, or if systematic (joints) –give rocephin (except if first month right due to kernicterus?)
- Salmonella?
- Guaiac?
- Blood or not blood game – Very hard to know the difference
- Take home points:
- Is it really blood?
- Causes: upper lower, age, severity
- Management varies, stabilize first
- Differential diagnosis by age summarized
- Normal vitals by age
- Additional resources:
- GI Bleeding in Children (PEMPlaybook)
Ivan – Resident Lecture—Cyanide/CO poisoning
- Cyanide
- Rapidly increase lactic acid
- Can → early parkinson’s (damage to basal ganglia)
- Sources:
- NaCN (gold mining)
- KCN (jewelry cleaner/buffer)
- CACN
- Cyanogens include cyanide glycosides (food or “natural) e.g amygdalin
- Tangent 1: How much nitroprusside to kill your patient?
- 10-15mcg/kg/min for >1 hour
- Half life 11 minutes
- 0.3 mic/minute -starting rate
- Symptoms
- TRIAD: AMS, Hypotension, Elevated lactate (BOARDS Q!)
- Non-reactive mydriasis
- Smell = bitter almonds (BOARDS Q!)
- Diagnostics–
- PULL LABS PRIOR TO GIVING CYANOKIT
- Cyanide level (takes too long, just treat)
- Lactate
- Carboxyhemoglobin
- ABG vs VBG (<10% difference, may be a myth?)
- Pulse ox
- CO false readings
- Cyanohemoglobin is another one of those “myths” ~~ usually normal pulse ox read
- Treatment
- ABC, Airway, O2
- Cyanokit (Hydroxycobaline)
- May turn urine bright red
- Case report of interfering with hemodialysis
- Lilly kit (CAK)
- Amyl nitrite (poppers), sodium nitrite, sodium thiosulfate
- Side effects:
- Methemoglobinemia
- Tangent two:
- Hydrogen sulfide
- ‘Ten dead people in a sewer’ = HS
- Carbon monoxide
- Metabolic acidosis
- CO level is important for consideration for hyperbaric treatment
- Hyperbarics:
- Pregnancy with CO hemoglobin level >15%
- Fetal Hb tends to bind more CO
- Blood level >25%
- Pregnancy with CO hemoglobin level >15%
Jessica – Resident Lecture – Case Presentation
- Sign out from previous team: 34F with RUQ TTP, pending labs and US
- From Pakistan, in US for 10 years
- PMH eye problem with discharge, hearing loss
- Sx: back, hip, leg pain, generalized weakness; 2w n/v/d; 6 months purulent eye drainage
- LMP 1 month ago
- Incontinent of urine–was too weak to get up on exam.
- Increase in eye discharge on re-examination
- So what’s going on??
- Hearing loss, eye problem (6months), 2 weeks n/v/d, weakness
- DDx includes Guillain-Barre Syndrome
- CRP elevated
- Dx: Wegener’s (Granulmatossi with Polyangiitis)
- Symptoms: respiratory, kidney, lung
- Strokes, reduced vision/hearing, small vessel occlusions everywhere/hemorrhage-alveolar hemorrhage
- Tx: IV steroids
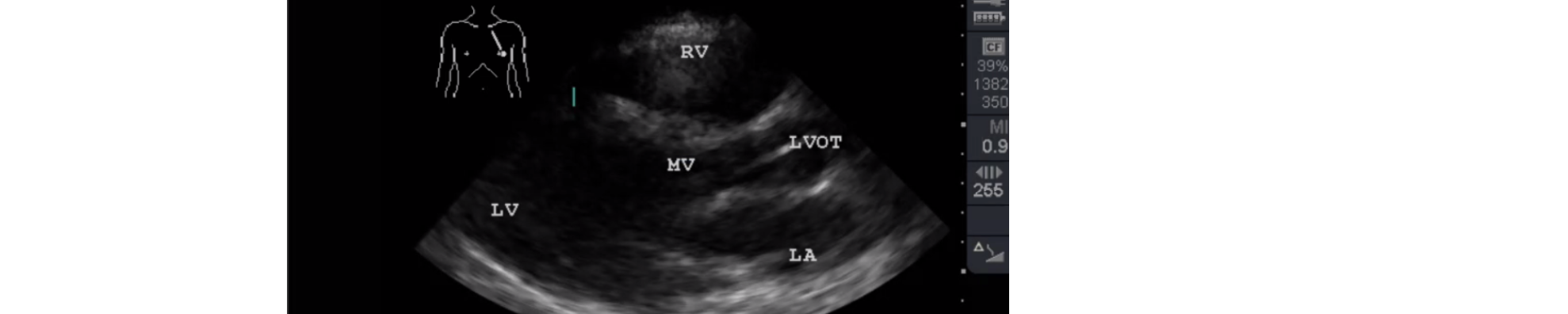
Jessica – Ultrasound
- Core Ultrasound
- Parasternal long view
- Parasternal short
- Apical 4 chamber
- Subxiphoid view
- Ultrasound case reviewed
- EPSS (to estimate EF)
- Pericardial effusion
- Pulmonary embolism
- D-sign
- Right heart strain / RV dilation
- Thrombi visualization
- McConnell sign
- Regional RV wall motion abnormalities
- Lung exam
- 3+ B-lines, LR 12 for CHF
- Case 1 – cardiac effusion
- Case 2 – pneumonia w/ B-lines
- Case 3 – CCB ingestion → poor contractility + ventricle dilation = cardiogenic shock
- Tx: charcoal, insulin, pressorsb
Faseeh – EKG/CCU #3
- Postponed to next week
Kaiser Permanente Physician Southern California (SCPMG) – Job Searches and CV writing w/ Q+A
- Kaiser located: California, Virginia, DC, Washington state
- Physician started and run
- SCPMG (for profit entity):
- Insurer + hospitals + medical group
- Pre-authorization is not needed for visits
- SCPMG partnership tract
- Eligible after 3 years of full-time employment
- Benefits:
- Lots of specifics, please see website
- Relocation up to $10,000 to Southern California
- Retirement plan: Retire at 30years of service get 50% of your salary back per year (other year options as well)
- San Diego EM market–very hard to get into
- Things to put on CV:
- Questions:
- Fellowships: Ultrasound
- Does emergency medicine have “office hours/time” like other specialties in kaiser?
- Four hours/week to finish charts
- How easy is it to relocate within the group?
- Moving from southern california to washington –VERY DOABLE
- San Francisco to Los Angeles — VERY DOABLE
- Bakersfield to San Diego — NOT DOABLE
- What does full time mean in Kaiser?
- Each franchise runs differently:
- San Diego shifts: 8h, 10h, 12h
- Full time: 1650 hours/year (national average 1640/year)
- Each franchise runs differently:
- How do new grads get treated in the ED first six months?
- Get extra help with note writing, don’t get paired with students/residents.
- Never on shift alone right away.
- CV how to stand out: write a cover letter
- Contacts:
- Dr. Adam Schwartz, head of EM at San Diego KP
- MIchael Truong, physician recruiter EM/UC
- michael.v.truong@kp.org
- 800-541-7946
- Laramier “Lara” Lopez
- laramier.lopez@kp.org
- 800-541-7946