Residency/Department Updates
- When order MTP, just check MTP, DO NOT order any RBC/PLT/PLTs separately
- Make sure ELOC patient have all their meds, hospital bed, diet, activity orders, etc
- Still need to write daily progress note (signout note “received care from previous team, patient in ELOC pending xyz”)
- 7a: Resident Lectures – Dima – Q1 Conference Review / Hamzah –
- 8a: Denise – EKG/CCU lecture #2 / Chirag – US lecture
- 9a: BREAK / Dr Rizzo – Seizures (not completed from last week)
- 10a: Dr Rizzo – October’s Quick Hits Podcast #4 – Acetaminophen interactions/HD + acetaminophen overdose/dental infections/MTP RABT score/Statins for STEMI/Cricothyrotomy tips+tricks
- https://emergencymedicinecases.com/em-quick-hits-may-2109/
- 11a: Dominic Desmond – CIR/SEIU – Resident only lecture on union benefits w. Q+A
- Dr Rizzo’s recommended review prior to seizure talk: (review at least 1 or 2 links please – we will discuss)
http://www.emdocs.net/treatment-of-seizures-in-the-emergency-department-pearls-and-pitfalls/
https://emergencymedicinecases.com/approach-resolved-seizures/
https://emcrit.org/pulmcrit/status-epilepticus-2/
https://www.emra.org/emresident/article/pediatric-seizure/
Resident Lectures – Dima – Q1 Conference Review – Kahoot
- Review of everything EM over the last few months
- Link to kahoot: HERE
Resident Lecture – Hamzah- Urology Emergencies
- Priapism
- Low Flow
- Decreased venous outflow → ischemia → PAIN
- More common than high flow
- Common causes (Peds): Sickle Cell Dz, Leukemia, ED medication
- High Flow
- Arterial inflow excess or Art outflow obstruction
- Compartment syndrome of the penis
- Less common
- Common causes: Arterial laceration, spinal trauma
- Management
- Systemic analgesia ineffective
- Dorsal penile nerve block
- Warm compresses
- Invasive techniques
- Phenylephrine (ɑ-adrenergic agonist) – 200-500mcg injection (in 1mL of NS) @ 2 & 10 o’clock position; can repeat q20 mins
- If ineffective, patient needs OR for possible surgical decompression (fasciotomy of the penis)
- Low Flow
- Testicular Torsion
- Background
- Most common cause of acute scrotal pain pre-puberty
- Twisting of spermatic cord → decreased blood flow → ischemia → necrosis
- Risk factors: Hx of cryptorchidism (Ivan will find them), horizontal testicular lie, younger
- Physical exam
- Unilateral tender firm testicle, erythema, edema, swelling, higher-riding testis, loss of cremasteric reflex on affected side
- “Time is testicle”
- TWIST score – not externally validated
- Do testicular exam on every acute RLQ pain (especially if peds, poor historian, wheelchair bound)
- Management
- Definitive: OR with Urology
- Do not delay consult for results (US, Labs, etc)
- Can consider manual de-torsion (~75% of torsions are internally rotated, so can “open the book” → Grasp testis and externally rotate towards anterolateral thigh)
- Intermittent torsion can occur
- Maintain level of suspicion even if negative ultrasound
- Torsion of testicular appendage, “blue dot” sign
- Background
- Phimosis
- Uncomfortable but not typically emergency (unless systemic infection)
- Non-retracted foreskin stuck over glans of penis
- Paraphimosis
- EMERGENCY
- Retracted foreskin trapped behind glans of penis
- Management
- Manual reduction
- Granulated sugar (to distal penis as an osmotic agent)
- Failure → urology consult for dorsal slit
- Fournier’s Gangrene
- EMERGENCY
- “Necrotizing fasciitis of the genital area”
- Life-threatening polymicrobial necrotizing skin/soft tissue of perineum, genitalia, or perianal areas
- Inciting event: typically some kind of urogenital trauma or source of infection (recently shaved, ingrown hair, etc)
- Most common risk factor: diabetes (also much more common in males)
- Physical exam
- Make sure to palpate! Look for crepitus
- Imaging
- CT may show soft tissue gas
- LRINEC score – not externally validated
- As with all scoring tools, this does not EXCLUDE these conditions; however it may increase the likelihood
- Management
- Surgical exploration is gold standard
- Consult urology & general surgery
- Early aggressive antibiotics (broad spectrum with Pseudomonas coverage – Meropenem & Vanc)
Denise – EKG/CCU lecture #2- Vtach
- Ventricular tachycardia
- Less than 3 ventricular beats in a row = PVCs
- More than 3 ventricular beats in a row = VT
- Non-sustained VT is <30 seconds
- Sustained VT is >30 seconds
- Differentials:
- SVT with aberrant conduction (WPW or BBB)
- Atrial Flutter
- Sinus Tachycardia with BBB
- MIMICS:
- HyperK (esp if QRS >200ms)
- Na-channel blocker OD (esp if QRS >200ms)
- Accelerated Idioventricular Rhythm
- 4 “flavors” of VT
- Monomorphic
- Classic
- Typically prior or current myocardial ischemia
- Polymorphic
- Usually related to ischemic event
- TdP
- Exercise induced
- Younger adults
- Catecholaminergic Polymorphic VT
- Congenital / hereditary cause of recurrent VT
- Resistant to many therapies
- DO NOT GIVE Amio or Procain → Rx: BB
- Monomorphic
- Wide and regular = ASSUME VTACH
- No algorithm good enough (Brugada)
- Assume its VT, treat for VT
- Treatment
- Put everyone on pads!
- Stable (with pulses, relatively normal BP)
- Procainamide (100mg q5 min)
- C/I in CHF, give amio instead
- Amiodarone (150mg over 10min, drip 1mg/min)
- Dr. Jeong: DON’T SLAM → hypotension
- Synchronized cardioversion
- If not synchronized → R-on-T phenomenon → vfib
- Procainamide (100mg q5 min)
- Unstable
- ⚡️⚡️⚡️
- Defibrillation (Can also try sync’d cardioversion → at worst, it’s unsync’d and ultimately the same as defib)
- Give magnesium too, it’s hard to distinguish between monomorphic and polymorphic and it won’t do harm – Dr. Rizzo
- Procainamide > Amio (Procainamide is 1st line for stable VT)
Chirag – US lecture – US of the Eye
- Case: 50M painless vision loss of R eye s/p punched in the face ~2-3 days prior
- VS of the eye: Pupils, EOM, Visual acuity, Visual fields, IOP (unless globe rupture)
- Direct visualization (fundoscopy)
- Operator dependent → EM <<< Ophtho
- Ocular US
- Reproducible, can save images and track changes
- Can evaluate anterior, middle, posterior chambers & optic nerve
- Dr. Rizzo – Make sure patient moves eye while doing US exam
- POCUS 101: Ocular US Guide
- US indications
- Eye pain
- Acute vision changes
- Trauma (**DO NOT US EYE if suspected globe rupture)
- ICP elevation
- Periorbital edema
- Lens dislocation
- US technique
- Use linear (vascular / high frequency) probe
- Tegaderm over the closed eyelid → LOTS of gel
- Have patient lay back with face parallel to ceiling
- Have patient look in all directions; scan through all planes
- Check other eye too
- Eye anatomy
- Eye irrigation pearls:
- pH of normal saline is 5.5, consider sterile water instead
- Morgan Lens irrigation is MESSY – prepare for a flood
- Anesthetize the eye before placing Morgan Lens
- Can consider using Nasal Cannula tubing over nasal bridge if intolerant of Morgan Lens
- Retinal detachment
- Macula on — STAT optho (surgical repair can restore vision within 24 hours)
- “(mac-on), central vision is preserved and emergent repair is essential before progression to a mac-off RD.”
- Retinal Detachment (jetEM)
- Macula off — outpatient follow up
- Macula on — STAT optho (surgical repair can restore vision within 24 hours)
- Lens Dislocation
- Previous cataract surgery can look like dislocated lens on US
- Elevated IOP
- Measure 3mm from posterior surface of retina, then across; if optic nerve >5mm then suggests increased IOP
- Retrobulbar hematoma
- Guitar pick sign
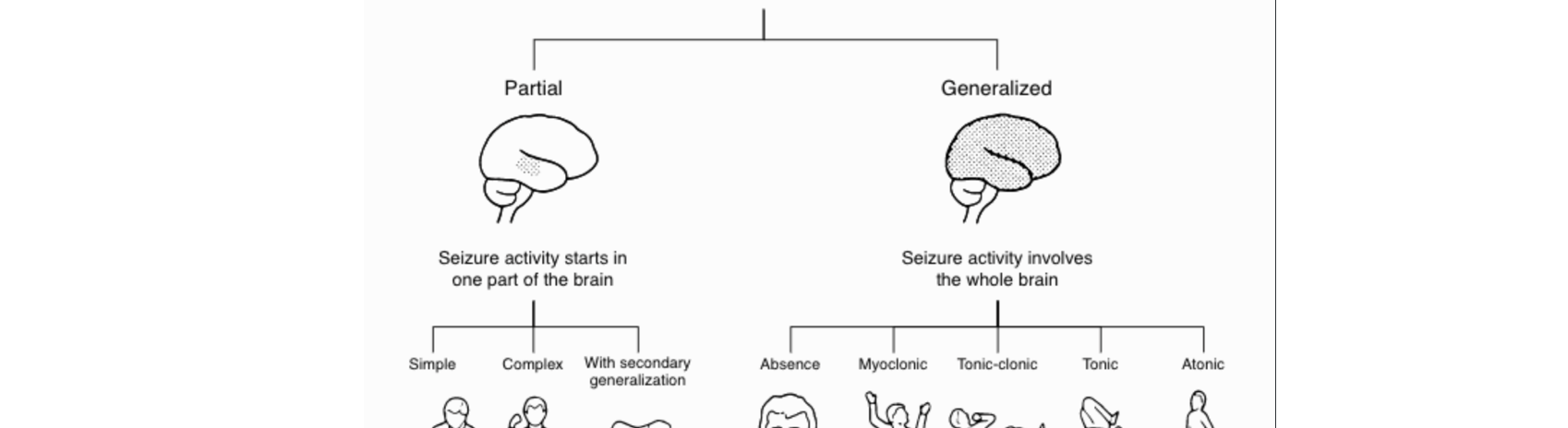
Dr Rizzo – Seizures (not completed this week either)
Resources for seizure discussion:
- Approach to Adult First Time Seizure in the ED (CoreEM)
- Treatment of Seizures in the Emergency Department: Pearls and Pitfalls – emDOCs.net – Emergency Medicine Education (EMDocs)
- Emergency Approach Resolved Seizure | EM Cases Podcast (EMCases)
- PulmCrit- Resuscitationist’s guide to status epilepticus (EMCrit)
- Management of Pediatric Seizures EMRA
- ESETT – The Bottom Line
Notes from Dr. Rizzo:
- Why talking about managing seizures is important:
- The longer the seizure continues, the more refractory it becomes to therapy. The duration of status epilepticus which may cause permanent brain damage is unknown, with experts currently suggesting thirty minutes
- Aside from the brain, persistent status epilepticus may cause aspiration, hyperkalemia, rhabdomyolysis, hyperthermia, myocardial infarction, and arrhythmia.
- Definitions
- Provoked (7 days from event?) vs unprovoked seizures
- History
- Questions that can help guide your ED management decisions:
- Is the patient back to his baseline neurological status? (get collateral info)
- Is this a first time seizure?
- Be aware that 50% of “first time seizures” have had prior events (multiple seizures in past consider starting meds)
- Consider Syncope!
- Is the seizure provoked or unprovoked?
- Questions that can help guide your ED management decisions:
- Differential diagnosis
- Vitals
- Tox(meds/withdrawal)
- Addiction
- Infectious
- Neuro
- Metabolic (hyponatremia = 2amps of HCO3- > hypertonic)
- Cardio
- Workup
- FS
- EKG
- CT
- EEG
- LP
- MRI
- Disposition
- first time seizure + back to baseline → no need for starting AED
- Status Epilepticus
- What else can be done?
- The combination of ketamine and propofol should theoretically provide synergistic anti-epileptic activity.
- Propofol stimulates the GABA receptors (the main inhibitory neurotransmitter in the brain)
- Ketamine inhibits NMDA receptors (a major excitatory neurotransmitter).
- The combination of these two effects causes a profound decrease in CNS activity. Ketamine combined with propofol (“ketofol”) was effective in published series of patients with super-refractory status epilepticus
- The combination of ketamine and propofol should theoretically provide synergistic anti-epileptic activity.
- Intubation
- Some consider it a failure
- Others consider it an important part of care that minimizes additional complications
- Early intubation with PROPER medications while intubated + paralysis concerns
Dr Rizzo – October’s Quick Hits Podcast #4 (LINK to EMCases)
Acetaminophen interactions/HD + acetaminophen overdose
- Tylenol + Warfarin interaction
- Tylenol increases INR, even small doses
- Doses of ~2g per day can cause INR to double
- APAP → Glucuronidation → NAPQI (toxic metabolite) → reduced by Glutathione → 😀
- Depleted Glutathione interferes with Vitamin K pathway leading to increased INR
- Tylenol increases INR, even small doses
- Massive tylenol ingestion
- 150 mg/kg = Toxic dose
- Consider MICU consult and emergent dialysis
- VBG may show acidosis, AMS (LFTs normal)
- Don’t just intubate for AMS and send to ICU
- Tylenol in general
- Need to 4 hour level, >150 = treat, <150 consider treating
- Consider charcoal if 1-2 hours after ingestion
Dental infections
- Pulpitis – inflammation, pain, hot/cold intolerance
- Definitive management: Dental evaluation
- Periapical abscess, can progress to ludwigs
- Usually no role for ABX in periapical abscess
Massive transfusion protocols RABT score
- MDCalc RABT Score
- RABT score (>2 = positive)
- Shock index > 1.0
- Pelvic Fracture
- Positive FAST
- Penetrating Injury
- Sensitivity 84%; Specificity 77%, NOT externally validated yet
Statins for STEMI
- Give Atorvastatin 80mg for all STEMIs
- “41% reduction in reinfarction going for PCI”
Cricothyrotomy tips+tricks
- HALO procedures (high-acuity, low-occurrence)
- Cricothyrotomy
- Resuscitative Thoracotomy
- Lateral canthotomy
- Resuscitative hysterotomy (perimortem c-section)
- Finger thoracostomy / Chest tube / Needle decompression
- Pericardiocentesis
- TVP placement
- Breech / Precipitous delivery
- Neonatal resuscitation
- Priapism drainage
- Mandible dislocation
- Bloody airway (SALAD, esophagus intubation, like Nancy last year, etc)
Dominic Desmond – CIR/SEIU – Resident only lecture on union benefits w. Q+A
- Learn about your union
- Lots of benefits — use them
- Mallory is our union rep