Residency Updates with Dr Jeong + Faculty
- “A person is smart, people are dumb” -Tommy Lee Jones, Men In Black
- Department getting busy, thanks for working hard
- You are responsible for your own education and your own patients
- Go to every resus, but don’t stay so long that it’s a detriment to your own team — find a balance
- Your plate should always be full, always be a little bit uncomfortable, always push yourself, write down things and look them up later when hangin’ at a coffee shop
- Be consistent — work hard with every attending
Dr. Kindschuh updates
- About half of radiology staff absent due to vaccination mandate
- Sepsis: Under national benchmark for compliance with 3-hour bundle (below 36%) ☹️
- Keep ordering radiology studies as you were doing previously
- However, these scans will have to be cleared by each attending
- Especially CT scans!
- Use decision rules to document why scans were not indicated (ex: Canadian Head CT)
- However, these scans will have to be cleared by each attending
- Don’t call CT tech unless its critical (time for red zone pts expected to be <90m to get scanned)
- Don’t do imaging as courtesy to IM team, unless it is not emergently indicated
- Administered Tenecteplase 6 times in month within the 30 minutes target
- Studies show outcomes are better if administered at <45 minutes
- How to order: type in “tenec” → facility list → order set
Residency news and updates:
- Envision physician recruiting gave us $50 grub hub gift cards. Information from Envision meeting at the bottom of the summary.
- 7a: Resident Lecture: Rob (please send me your topic) / Eugene – Troubleshooting the Complicated Central Line
- 8a: Denise CCU/EKG lecture #1 / BREAK
- 9a: Dr Seeram – DKA/HHS lecture
- 10a: Dr Rizzo – Everything you ever wanted to learn about catching a SEIZURE (Delayed – maybe next time)
- 1045a: Residency Updates with Dr Jeong + Faculty
- 11a: CLOSED residency meeting / CLOSED faculty meeting (Q1 review)
*Envision Group 12-1pm FREE $50 grubhub for every person for attending
Resources to read prior to seizure discussion:
- Approach to Adult First Time Seizure in the ED (CoreEM)
- Treatment of Seizures in the Emergency Department: Pearls and Pitfalls (EMDocs)
- Emergency Approach Resolved Seizure | EM Cases Podcast (EMCases)
- PulmCrit- Resuscitationist’s guide to status epilepticus (EMCrit)
- Management of Pediatric Seizures EMRA (EMRA)
- ESETT – The Bottom Line (The Bottom Line)
Eugene – Troubleshooting the Complicated Central Line
- Central line is NOT a resuscitative line, meaning the following:
- “No such a thing as a crash central line”
- Flow rates: Poiseuille law
- Contraindications:
- Absolute
- Infection over space
- Anatomic obstruction
- Site specific: subclavian – trauma/ipsilateral clavicle fracture or proximal ribs
- Relative
- Coagulopathy (don’t do if plt < 20k)
- Distortion of landmarks by trauma or congenital abnormalities
- Prior vessel injury or procedures
- Morbid obesity (lol)
- Combative patient
- Absolute
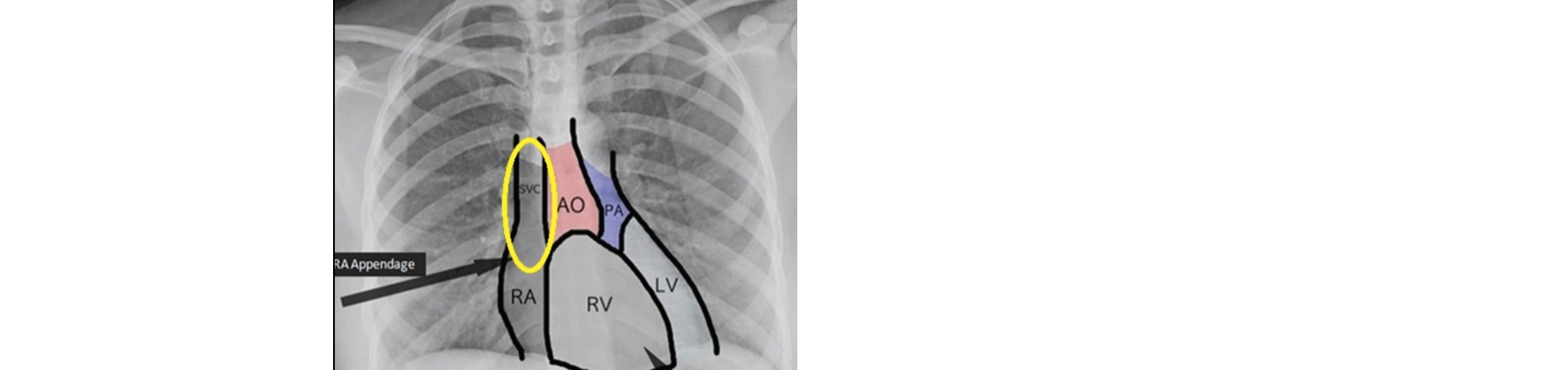
- Central line placement confirmation (should be in yellow circle – “cavo-atrial junction”)
- 14, 15, 17, 18 Rule
- 14 R subclav, 15 RIJ, 17 L subclav, 18 LIJ
- But actually:
-
- Anatomical variation – Persistent left SVC
- 0.3% of population has “persistent L superior vena cava”
- Troubleshooting
- Blood aspirate through all lumens
- Is blood venous? → ALWAYS GET VBG TO CONFIRM PLACEMENT
- VBG vs ABG (LITFL)
- Convert VBG to ABG (PulmCrit)
- Transducer waveform consistent with a CVP waveform
- Catheter on CXR consistent with placement within a central vein and not kinked?
- CL wire – put J (hooked) portion facing medially when doing IJ – higher success rate
- Also with Subclavian, higher success rate if J portion faces inferiorly
- Syringeless CVC placement with catheter (EMRAP)
- Subclavian tips
- 3SITES trial – Complications of CL by site
- Intravascular Complications of Central Venous Catheterization by Insertion Site – 2015
- More infections and DVT with femorals, more PTX with subclavians (actually less infections/DVTs with subclavians though)
- Other trials opposing 3SITES
- Cumulative Evidence of Randomized Controlled and Observational Studies on Catheter-Related Infection Risk of Central Venous Catheter Insertion Site in ICU Patients: A Pairwise and Network Meta-Analysis – 2017
- The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis – 2012
- PS – ped CL sizes
- Scott Weingart CVC pro-tips video (15 min)
Resident Lecture: Rob – Obesity
- BMI = weight (kg) ÷ height (m)
- Super obese (actual ICD 10) is BMI > 50
- Pulmonary changes in obesity:
- Restrictive physiologic pattern 2/2 reduction in chest wall compromise
- —> reduces lung volumes and increased airway resistance
- Fibrosis from chronic airway changes
- Respiratory muscles have increased workload and oxygen consumption
- Intrapulmonary shunting
- V/Q mismatch
- Shorter safe apnea time → decreased respiratory reserve
- Restrictive physiologic pattern 2/2 reduction in chest wall compromise
- Circulatory changes
- Hyperdynamic circulation – increased intravascular volume
- LVH
- LV diastolic dysfunction
- RV dysfunction
- ⇧ pulmonary HTN
- ⇧ systemic pressure
- ECG alterations in obese patient:
- Low voltage
- LVH
- ⇧ QT (rarely >500ms due to obesity alone)
- Pulmonary / R sided strain due to ongoing restrictive airway changes
- Hematologic changes
- Prothrombotic (inc blood viscosity)
- ⇧ fibrinogen
- ⇧antithrombin 3
- ⇧ plasmin activator inhibitor levels
- ⇩ fibrinolysis
- GI
- Inc risk of aspiration
- Increased intra-ABD pressure @ baseline
- Vital signs
- Automated BP cuff measures MAP (monitor then extrapolates to get SBP/DBP)
- BP cuff can overestimate BP (too small)
- Borderline BP could represent a shock state in an obese adult
- Consider placing an early arterial line to obtain and trend bp
- Shock index can be helpful; SI = HR/SBP
- Intubation
- Setup is MORE IMPORTANT – See below for BIGRAMP
- Rizzo Tips Korner: Use PEEP VALVE when giving BVM breaths (mask or ETT)
- RSI drugs – which use TBW vs IBW
- Dr. Jeong’s Corner:
- Prior discussion on The Crashing Obese Patient
Denise CCU/EKG lecture #1 – Post Cardiac Arrest Care
- PulmCrit / IBCC Chapter: Post-Arrest Care (PulmCrit)
- Post Cardiac Arrest Syndrome (Post Resuscitation Syndrome)
- Ischemic reperfusion injury in multiple organ systems
- Hypoperfusion → pan-organ ischemia → increased metabolic demand
- Lazarus Phenomenon
- Spontaneous ROSC following termination of resuscitative efforts – could be in resus room, hallway, body bag, morgue, Ivan’s basement, etc (hours up to a day or two later)
- Lazarus syndrome – Wikipedia
- Post-cardiac arrest myocardial dysfunction:
- Initially hyperkinetic (catecholamines) then global hypokinesis – 72 hours
- Systemic ischemia/reperfusion: similar to septic shock
- Cardiac arrest causes: H’s and T’s (from Osmosis)
- Hypothermia vs normothermia after cardiac arrest
- TTM1: no difference between hypothermia vs normothermia – in 2013
- Summary: No difference (but too narrow a study to generalize to population)
- TTM2 2021 on hypothermia on OHCA
- Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest
- TLDR: In patients with coma after out-of-hospital cardiac arrest, targeted hypothermia did not lead to a lower incidence of death by 6 months than targeted normothermia
- PulmCrit Discussion of Hypothermia & TTM2 Study (PulmCrit)
- TTM1: no difference between hypothermia vs normothermia – in 2013
- Glycemic control post-cardiac arrest: (NICE-SUGAR Study)
- PANSCAN after cardiac arrest
- Rizzo corner: Head CT after cardiac arrest (2021)
- Utility of Abnormal Head Computed Tomography in Predicting Outcome in Out-of-Hospital Cardiac Arrest Victims | Therapeutic Hypothermia and Temperature Management
- TLDR: CT head post cardiac arrest demonstrating cerebral edema, ischemia, something bad→ worse prognosis
- Utility of Abnormal Head Computed Tomography in Predicting Outcome in Out-of-Hospital Cardiac Arrest Victims | Therapeutic Hypothermia and Temperature Management
- Prognosis
- Neuroprognostication after Cardiac Arrest (PulmCrit / IBCC)
- Brain stem reflexes (pupillary, corneal, best motor response at 72 hours)
- Presence of myoclonic status epilepticus
- NSE: neuron-specific enolase > 33 mcg.L at 1-3 days
- EEG/SSEP
- Apnea test
- CT/MRI
Dr Seeram – DKA/HHS lecture
- DM1: Autoimmune/idiopathic destruction of beta cells, so no insulin
- DM2: Insulin deficiency and/increased resistance
- DKA/HHS: Similar disease processes – Both can occur in type 1 and type 2 DM
- DKA (PulmCrit / IBCC Chapter: DKA), (Deranged Phys: Diabetic ketoacidosis)
- Typically T1DM
- Tends to be lower blood sugar (≦250)
- More common in younger (<65)
- Fluid deficit ~6L
- Usually faster onset (hours to days) → insulin deficiency → ketogenesis → dehydration
- YES ketoacidosis, not usually hyperosmolar
- Sx:N/V, ab pain, dehydrated (fluid deficit ~6L), tachypnea, less likely to have a fever
- DKA (PulmCrit / IBCC Chapter: DKA), (Deranged Phys: Diabetic ketoacidosis)
- HHS (PulmCrit / IBCC Chapter: HHS) (Deranged Phys: Hyperosmolar non ketotic hyperglycaemic coma (HONK))
- Typically T2DM
- Tends to be higher blood sugar (500+)
- More common in older (>65)
- Fluid deficit 8-10L
- Usually slower onset (days to weeks) → Insulin presence prevents significant ketogenesis → Severely elevated FSBS (case reports of up to 2400mg/dL) → PROFOUND dehydration
- NO ketoacidosis, YES hyperosmolarity
- Sx: Neuro Sx, AMS, confusion, stupor, lethargy, seizures, neuro deficits possible, profound dehydration (~8-10L), less likely to mount a fever
- Lab Findings in DKA/HHS
- Pseudo-hyponatremia (dilution of serum sodium with Glucose)
- TLDR: for every ↑100 glucose → ↑1.6 sodium
- Hyperkalemia
- Serum K is normal or elevated
- Total body K deficient
- Pseudo-hyponatremia (dilution of serum sodium with Glucose)
- Labs in DKA/HHS
- Euglycemic DKA
- Often seen with SGLT2 (_____flozin) inhibitors (BOARD QUESTION)
- These medications cause patients pee out their excess blood sugar (above ~100mg/dL)
- Treatment is same as DKA, except you start on dextrose-containing fluids at the beginning
- DKA TREATMENT
- IV Fluids
- PulmCrit / IBCC Chapter: Fluid Selection & pH-guided Fluid Resuscitation
- ALWAYS use Lactated Ringers (balanced solution, closer to physiologic)
- “There is nothing normal about normal saline” – everyone
- Avoids hyperchloremic metabolic acidosis
- Typically give 1-2 L bolus (LR, because NS is poison)
- UpToDate: 20mL/kg/hour for the first few hours
- Maximum: 50cc/kg over first 4 hours
- PulmCrit- Get SMART: Nine reasons to quit using normal saline for resuscitation
- Insulin
- Check potassium first
- K <3.3 → replete potassium first, stop insulin
- K 3.3-5.3 → give insulin with potassium
- K >5.3 → just insulin
- Insulin dose: 0.1mg/kg/hr
- If glucose doesn’t drop 50-70mg/dL in the first hour, DOUBLE insulin gtt
- Check potassium first
- Episode 29 – Hyperglycemia (FOAMCast)
- DKA protocol with long/short acting insulin from Montefiore medical center
- IV Fluids
- HHS TREATMENT
- VERY similar to DKA treatment
- NOT chasing ketosis
- MUCH SLOWER → Took the patient days-weeks to get there, need to drop osmolality slowly to avoid worsening cerebral edema
- End goal: Normalize serum OSM & improved mental status
- Sending a mild DKA pt home:
- Need to bridge with long acting minimum of 2 hours prior to discontinuing insulin gtt
- Tolerating POs
- Side note: even ICU pt’s – diet early; Early vs late oral nutrition in patients with diabetic ketoacidosis admitted to a medical intensive care unit
- ALSO: can give pt’s home dose of long acting insulin upfront to smooth blood sugar drop while on insulin gtt
- PulmCrit – Early basal insulin in DKA
- Dr. Jeong’s Corner: Bicarb indications?
- Generally, no
- If huge amount of diuresis/diarrhea, YES cuz losing bicarb
- Indicated with pH very low (pH <7.1)
- Considerations for using Bicarb in DKA: Dominating the Acidosis in DKA (PulmCrit)
- Intubation
- DONT (if you can avoid it)
- Hard to compensate for increase RR on when on the vent → acidosis can worsen → badness
- Weingart: EMCrit 3 – Laryngoscope as a Murder Weapon (LAMW) Series – Ventilatory Kills – Intubating the patient with Severe Metabolic Acidosis
- Consider BiPAP as pre-oxygenation
- Indications for intubation may include:
- Airway protection
- Emergent surgical indication (example: DKA + perforated viscus)
- Respiratory arrest or impending arrest
- Intubation notes
- Large ETT
- Set initial RR ~30
- WATCH CLOSELY
- Cerebral edema
- More common in children
- High mortality (20%)
- Tx: Hypertonic saline, mannitol
- Links from Dr. Jeong
- C3 – DKA: Approach to The Critical Patient
- Diabetic Ketoacidosis (DKA) (EMCrit)
- PulmCrit- Dominating the acidosis in DKA
- Awesome Talks by Sara Crager on Acidosis in DKA
Dr Rizzo – Everything you ever wanted to learn about catching a SEIZURE
(DELAYED DUE TO ACUTE-ON-CHRONIC TIME MANAGEMENT DIFFICULTIES)
Resources for seizure discussion:
- Approach to Adult First Time Seizure in the ED (CoreEM)
- Treatment of Seizures in the Emergency Department: Pearls and Pitfalls – emDOCs.net – Emergency Medicine Education (EMDocs)
- Emergency Approach Resolved Seizure | EM Cases Podcast (EMCases)
- PulmCrit- Resuscitationist’s guide to status epilepticus (EMCrit)
- Management of Pediatric Seizures EMRA
- ESETT – The Bottom Line
Notes from Dr. Rizzo:
- Why talking about managing seizures is important:
- The longer the seizure continues, the more refractory it becomes to therapy. The duration of status epilepticus which may cause permanent brain damage is unknown, with experts currently suggesting thirty minutes
- Aside from the brain, persistent status epilepticus may cause aspiration, hyperkalemia, rhabdomyolysis, hyperthermia, myocardial infarction, and arrhythmia.
- Definitions
- Provoked (7 days from event?) vs unprovoked seizures
- History
- Questions that can help guide your ED management decisions:
- Is the patient back to his baseline neurological status? (get collateral info)
- Is this a first time seizure?
- Be aware that 50% of “first time seizures” have had prior events (multiple seizures in past consider starting meds)
- Consider Syncope!
- Is the seizure provoked or unprovoked?
- Questions that can help guide your ED management decisions:
- Differential diagnosis
- Vitals
- Tox(meds/withdrawal)
- Addiction
- Infectious
- Neuro
- Metabolic (hyponatremia = 2amps of HCO3- > hypertonic)
- Cardio
- Workup
- FS
- EKG
- CT
- EEG
- LP
- MRI
- Disposition
- first time seizure + back to baseline → no need for starting AED
- Status Epilepticus
- What else can be done?
- The combination of ketamine and propofol should theoretically provide synergistic anti-epileptic activity.
- Propofol stimulates the GABA receptors (the main inhibitory neurotransmitter in the brain)
- Ketamine inhibits NMDA receptors (a major excitatory neurotransmitter).
- The combination of these two effects causes a profound decrease in CNS activity. Ketamine combined with propofol (“ketofol”) was effective in published series of patients with super-refractory status epilepticus
- The combination of ketamine and propofol should theoretically provide synergistic anti-epileptic activity.
- Intubation
- Some consider it a failure
- Others consider it an important part of care that minimizes additional complications
- Early intubation with PROPER medications while intubated + paralysis concerns
Envision meeting
- Envision: www.envisionphysicianservices.com
- Physician staffing company, physician lead
- Located in 45 states
- Practical tips for obtaining jobs:
- Keep all your ATLS, PALS, etc. certificates with you & up to date
- FSMB | Federation Credentials Verification Service (FCVS) keeps all of your documents in one place so you can apply for multiple jobs without reaching out to every place to get paperwork from
- Salaries:
- Varies by site & physician group
- Upstate NY: $210-$230/days +$20 night differential; 120hrs/month
- Part time work available?
- Depends on site and need
- 94% retention rate with physicians hired, physicians usually leave the group when they move to a different area of the country (Florida, California)
- Loan forgiveness/assistance programs: none.
- Signing bonuses: ‘case by case basis: there are some exceptions’
- Noncompete clauses:
- Nonsolicitaiton: ‘Please do not participate in trying to steal your contract from the hospital and starting your own group’ “Please do not solicit our employees”
- Hospital specific: mile radius, time frame of employment
- Fellowships
- PEM offered through Morristown hospital
- EMS, US offered through Envision in New Jersey
- Contact information
3