Residency news and updates:
- Wednesday, September 29, 2021 at 12:00pm: Envision Health info service.
- Residents get $50 uber eats gift card for attending; if you have not Click Here to RSVP e-mail kristi.thetford@envisionhealth.com with any questions.
Dr. Kindschuh Updates:
- Joint commission is here already
- Consent for EVERYTHING (procedures, AMA, etc) in appropriate language
- 7a: Geoff / JP (TRI) – resident lectures (BJ postponed)
- 8a: Dr Sun – Hyperkalemia / Faseeh – CCU lecture #2
- 9a: BREAK / Dr Jeong – C3 – Asthma/COPD
- 10a: Dr Jeong – C3 – Asthma/COPD
- 11a: Dr Rhodes – Pediatric asthma
Resources for this week:
- EMRAP C3 Part I – The Crashing Asthmatic C3 – The “Crashing” Asthmatic
- EMRAP C3 Part II – The Stable Asthmatic C3 – The “Stable” Asthmatic
- EMRAP C3 – Asthma.pdf (written summary)
- EMCRIT Acute exacerbation of COPD – Acute exacerbation of COPD (AECOPD)
- EMCRIT Asthma – Asthma
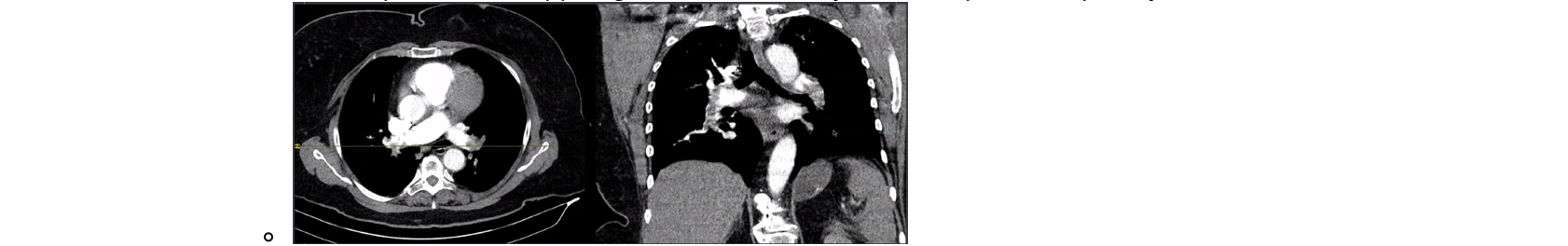
Geoff – Syncope – “They Done Fell Out”
- EKG = sinus tachycardia, rate ~100, FS 200s
- DDx: AS, PE, PNA, Vasovagal, Seizure, MI, stroke
- Conclusion: PE
- ED team considered inhaled pulmonary vasodilator (nebulized NTG), but cautioned by Ophtho to avoid nitric oxide (Not the same, but what NTG is broken down into in bloodstream) due to potential for expansion of trapped gas — bubble in eye could expand and pt may lose vision
- FS 120, EKG = RBBB rate 100
- DDx: aortic dissection, MI
- Had a TVP in CCU in past, not PPM, planned for outpatient follow up for pacemaker
- Case continued… pt became unresponsive, intubated in between his unresponsive episodes, TVP placed by cardio in ED, discharged on hospital day 4, neuro intact, w/ brand new shiny PPM
- Syncope definition: brief LOC and postural tone that resolves spontaneously
- ~10 seconds of interrupted blood flow to brain/brainstem
- Near syncope = syncope (risks/outcomes)
- General Syncope workup:
- Blood sugar, ECG
- ACTUAL cardiac monitoring (in tele bed at end of red zone)
- Other labs and imaging on underlying conditions/MC etiology
- trop…
- Cardiac + neuro syncope has worse survival outcomes
- PE is NOT super common in patients that return back to baseline
- PESIT trial disproven – Quick PESIT update
- Predicting Dysrhythmias After Syncope (RebelEM)
- Author conclusions: Help identify High vs low risk
- Canadian Syncope Risk Score (externally validated, SF syncope rule is not)
- San Francisco Syncope Rule: “CHESS” (not externally validated) (will be on inservice)
-
-
- “Syncope AND _____”
- Links from Dr. Jeong
BJ – resident lectures –postponed
JP Fernandez – visiting TRI – Eclampsia
- DDx: IIH, posterior stroke, venous sinus thrombosis, ICH, electrolytes
- Continued ED course:
- Pt has seizure
- Further hx: vaginal delivery 19 weeks ago
- UA: 3+ proteinuria
- CTh negative, treated with IV mag
- Pre-eclampsia:
- new onset HTN w/ end organ damage – proteinuria (not necessary – ACOG 2013), thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, cerebral or visual symptoms
- Eclampsia: pre-eclampsia + seizures
- HELLP: hemolysis, elevated liver enzymes, low platelets
- Risk factors:
- DM, Hx of pre-eclampsia, multiple gestation, chronic HTN, CKD, autoimmune disease
- High risk pregnancies tx: prophylaxis low dose ASA
- Work up:
- UA, uric acid, CBC, LFTs, LDH
- CTH (if you do it): cerebral edema, diffuse white matter low-density areas, patchy area of low density, occipital white matter edema
- MRI: b/l hyperintense on T2; hypointense on T1 w/o diffusion restriction – mostly posterior cerebral circulation – most MRI findings are reversible
- After 34 weeks (pre-eclampsia w/ severe features) – steroids and deliver

- Eclampsia hypertension treatment?
- Labetalol
- Hydralazine
- Nifedipine
- Dr. Rizzo Magnesium facts:
- “Adverse effects of magnesium sulphate come largely from its action as a smooth muscle relaxant. The most serious are respiratory depression, and respiratory and cardiac arrest. However, the adverse effects follow a dose response. Deep tendon reflexes are lost at a serum magnesium level of 10 mEq/L, with respiratory depression occurring at 15 mEq/L and cardiac arrest at more than 15 mEq/L. “Using magnesium sulphate, rather than diazepam, more than halves the RR of recurrence of seizures (seven trials; 1390 women; RR 0.43, 95% CI 0.33 to 0.55). This means that, on average, for every seven women treated with magnesium sulphate rather than diazepam one recurrence of seizures will be prevented (NNT 7; 95% CI 5 to 9 women).”
- Think about postpartum eclampsia
- Can occur even 12weeks after birth
Dr Sun – Hyperkalemia

- Brady DDx: DIE – drugs, ischemia, electrolytes
- Drugs: brady bunch – BCCD – B-blockers, CCBs, Clonidine, Dig
- Ischemia: MI
- Electrolytes: Geoff’s actual favorite – BRASH
- EKG/labs
- Repeat EKG
- Hyperkalemia causes:
- Hyperkalemia clinical symptoms: non-specific
- Neuromuscular:weakness, fatigue, paralysis, lethargy, confusion
- Cardiac: arrhythmias, conduction abnormalities
- Bad for the heart: hyperK depolarizes cell membrane potential and decreases resting membrane potential, slows conductions
- Hyperkalemia EKG changes:
- ECG does not always progress in this way; per Amal Mattu “HyperK does whatever it wants”
- Also, it’s the rate of rise in K, not the absolute number (chronic elevation in the 7’s in HD patients could be lethal for pts with normal renal function)
- Retrospective review of the frequency of ECG changes in hyperkalemia (PubMed) – EKG changes poor sensitivity/specificity for hyperK
- Severe Hyperkalemia: Can the Electrocardiogram Risk Stratify for Short-term Adverse Events? (PubMed)
- HD – Electrolyte Emergencies (EMRAP video)
- HyperK ECG examples:
- Treatment
- Calcium chloride vs Calcium gluconate
- CalCl 3x stronger than Calcium Gluconate “Gluconate is Gooder for the veins”
- CaCl → sclerotic to veins
- Insulin & Dextrose
- Give 5u Insulin + 25g D50
- Albuterol – requires a lot of albuterol….
- Epinephrine
- Works like Albuterol (B2 agonist)
- Consider use if hypotensive or bradycardic
- DO NOT USE SALINE FOR HYPERKALEMIA
- There is nothing “normal” about normal saline
- Worsens acidosis, shifts MORE potassium out of cells to counteract acidosis, large chloride load, worse outcomes in almost all populations
- At the end of the day, water with salt in it should be reserved for making pasta
- Bicarb

- Bicarb pushes (hypertonic / crash cart Bicarb) DO NOT WORK
- Bicarb Drips DO WORK (if used in the correct patient populations)
- Consider using isotonic Bicarb drip as initial fluid resuscitation if hypovolemic
- Lokelma (oral potassium binding resins) → KayExelate is OUT
- Lowers K by ~0.2mM in the first 4 hours or ~0.4mM in the first 24 hours
- Emergency Potassium Normalization Treatment Including Sodium Zirconium Cyclosilicate: A Phase II, Randomized, Double-blind, Placebo-controlled Study (ENERGIZE)
- ALTERNATIVE OPTION – Kaliuresis (faster than Lokelma)
- Hemodialysis → If patient is ESRD on HD, get the wheels in motion EARLY
- Definitive treatment
- Can lower by 1mM per hour of HD (K of 8.0 → 5.0 after ~3hrs of HD)
- Dr. Rizzo comments:
- LOKELMA: Sodium Zirconium Cyclosilicate (SZC) is an oral potassium binder, essentially an upgrade of sodium polystyrene sulfonate (Kayexalate). Unlike sodium polystyrene sulfonate, SZC doesn’t appear to cause bowel necrosis.
- EW
- SZC is studied predominantly for subacute to chronic reduction in potassium. However, it does appear to cause some reduction in potassium levels acutely (perhaps ~0.2 mM within 4 hours, and ~0.4 mM within 24 hours).
- Potential side effects of SZC include constipation, hypokalemia, and volume overload (each 10 gram dose contains ~800 mg of sodium). None of these appear to be particularly common. Side-effects seem to be more problematic when the drug is taken chronically (particularly, hypokalemia or volume overload
- LOKELMA: Sodium Zirconium Cyclosilicate (SZC) is an oral potassium binder, essentially an upgrade of sodium polystyrene sulfonate (Kayexalate). Unlike sodium polystyrene sulfonate, SZC doesn’t appear to cause bowel necrosis.
- PEARLS
- Regarding Calcium dosing / redosing:
- From Dr. Rizzo, via EMCrit HyperK
- IV calcium is indicated for patients with EKG changes or a potassium >6.5 mM.(32852924)
- Initial dose:
- Peripheral access: 3 grams IV calcium gluconate over 10 minutes.
- Central access: 1 gram IV calcium chloride over 10 minutes or slow IV push.
- Further doses of calcium may be indicated for persistent, dangerous arrhythmias (e.g. ongoing bradycardia with hypoperfusion). Additionally, calcium only lasts for about 30-60 minutes, so the dose may need to be repeated.
- The ideal strategy for re-dosing is unknown. An expert guideline recommended re-dosing once or twice if needed, while admitting the lack of evidence.(28976587)
- Hyperkalemia is generally more dangerous than hypercalcemia, so you’re probably better off erring on the side of hypercalcemia. If you have a point-of-care electrolyte monitor (AKA iSTAT) available, check calcium levels and avoid pushing the ionized calcium >3mM.
- From Ivan:
- “Dr Smith blog… if patient has preexisting LBBB and concern for qrs widening with hyperK, obvi compare to prior ECGs, but essentially if QRS > 190 then there is something more going on then just LBBB”
- Hyperkalemia in the setting of Left Bundle Branch Block
- From Dr. Rizzo, via EMCrit HyperK
- Hyperkalemia – EMCrit Chapter & Podcast on HyperK
Faseeh – CCU lecture #2 – “bundles of joy”
- LBBB
- Criteria for LBBB
- QRS >0.12 sec
- Broad monomorphic R waves in I and V6 with no Q waves
- Broad monomorphic S waves in V1, may have a small r wave
- Side note: There is a more stringent LBBB definition when considering people for CRT-D – this includes the mentioned R wave peak time (>60 ms) in V5-V6
- R wave peak time, also known as intrinsicoid deflection, is the time from onset of earliest Q wave or R wave to the peak of the R wave in the lateral leads (aVL, V5-6)
- Side note: There is a more stringent LBBB definition when considering people for CRT-D – this includes the mentioned R wave peak time (>60 ms) in V5-V6
- “Appropriate discordance” = not pathologic
- Generally speaking (in a normal EKG):
- Concordance (QRS & T waves pointed the same direction) = good
- Discordance (QRS & T going opposite ways) = bad
- Example of LBBB with concordant STD: (STEMI equivalent)
- RBBB
- QRS duration > 120ms
- RSR’ pattern in V1-3 (“M-shaped” / “Bunny Ears” QRS complex)
- Wide, slurred S wave in lateral leads (I, aVL, V5-6)
- LAFB
- Left axis deviation (usually -45 to -90 degrees)
- qR complexes in leads I, aVL
- rS complexes in leads II, III, aVF
- Prolonged R wave peak time in aVL > 45ms
- LPFB
- Right axis deviation (RAD) (> +90 degrees)
- rS complexes in leads I and aVL
- qR complexes in leads II, III and aVF
- Prolonged R wave peak time in aVF
- Brugada
Dr Jeong “Core Content” Monthly Lecture – C3 – Asthma/COPD
Resources for this week:
EMRAP C3 Part I – The Crashing Asthmatic C3 – The “Crashing” Asthmatic
EMRAP C3 Part II – The Stable Asthmatic C3 – The “Stable” Asthmatic
- EMRAP C3 – Asthma.pdf (written summary)
EMCRIT Acute exacerbation of COPD – Acute exacerbation of COPD (AECOPD)
EMCRIT Asthma – Asthma
- Labs for Asthma vs COPD
- Asthma: don’t really need labs/CXR
- COPD: probably should get labs – high incidence of PNA in COPD exacerbations
- Antibiotics for COPD
- Are antibiotics beneficial for flare-ups of chronic obstructive pulmonary disease? (side note – cochrane review)
- Labs: Lactate (can go up with beta-agonist), PCT
- Peds Per Dr. Weber:
- “In pediatrics you do not need labs even if placing a line. Only obtain at that point if there’s a specific other diagnosis you’re working up. The pediatric inpatient team, even PICU, should not require labs for admission.”
- Peds Per Dr. Weber:
- Peak flow
- Use of Peak Expiratory Flow Rate Monitoring for the Management of Asthma in Adults in the Emergency Department
- If you need support for admission
- Dr. Radeos links
- https://www.ncbi.nlm.nih.gov/books/NBK7232/pdf/Bookshelf_NBK7232.pdf
- “Ensure saturation is 88-92% so patients don’t lose their hypoxic drive”
- Oxygen-induced hypercapnia in COPD: myths and facts – some people say that actual hypoventilation from high oxygen given to COPD is more due to hypoxic pulmonary vasoconstriction, and not hypoxic respiratory drive as previously thought…
- Consider AeroGen for the sicker asthmatics
- Why just 3 ipratropium and then only albuterol?
- Max out anticholinergic effects after 1.5mg (3x Ipratropium)
- Why is Atropine contraindicated in Asthma?
- Dose required of Atropine would excessively dry out mucus plugs in airways
- Steroid compared
- Steroid Conversion Calculator
- Decadron:
- PO shorter acting
- IM longer acting
- Prednisone
- Make sure to prescribe q12 hours not q24 hours
- Magnesium
- High-Dose Magnesium Sulfate Infusion for Severe Asthma in the Emergency Department: Efficacy Study
- 50 mg/kg over 1 hour (bolus) or high-dose prolonged magnesium sulfate infusion of 50 mg/kg/hr for 4 hours (max, 8.000 mg/4 hr)
- for non-infectious mediated asthma, expedites discharges from the emergency department with significant reduction in healthcare cost.
- Magnesium Sulfate for Asthma Attack – TheNNTTheNNT (The NNT)
- Dr. Rizzo: Mag is all benefit, no harm, just give it
- High-Dose Magnesium Sulfate Infusion for Severe Asthma in the Emergency Department: Efficacy Study
- Epinephrine
- IV vs IM
- We do IM, should probably do IV
- BIPAP/CPAP
- BiPAP: start 10/5
- There is an argument for CPAP; Dr. Dubey (MICU) has used HIGH settings (25/20) & had good results (Asthma physiology is obstructive, just like sleep apnea – trial of high settings could prevent intubation)
- PulmCrit- Mastering the dark arts of BiPAP & HFNC
- Intubation
- LAST thing you want to do
- Try BIPAP + Ketamine first (dissociative dose), if it fails → intubate
- Our BiPAPs can run as external ventilators (Tell RT you want to run as AVAPS / run with backup rate) to preoxygenate
- The Crashing Asthmatic / Intubation
- Back up intubation methods at bedside
- Big tube (at least 8.0, 8.5-9 if taller)
- Most experienced intubator
- Vent settings
- PRVC
- Note the LOW respiratory rate
- High I:E ratio ([normal I:E ~1:2] Aim for I:E >1:4 → PROLONG EXPIRATORY PHASE)
- Avoid breath stacking – look at flow waveform
- Permissive hypercapnia
- Asthma (EMCrit – initial settings)
- Plateau pressure <30 (peak pressure? Don’t worry about it)
- Pplat = pressure actual alveoli are seeing
- Ppeak = highest pressure in the system (can be 2/2 obstruction, biting tube, etc)
- CODING ASTHMATIC
- Breath stacking
- Remove the vent from ETT
- Decompress the chest → bilateral chest tubes
- PRVC – asthmatics have high intrathoracic pressures, so PRVC (Pressure regulated) sometimes won’t even deliver a breath because out of the pressure parameters – use VC
- PulmCrit – The Crashing Asthmatic with Leo Stemp
- This is a bleeding edge topic & not supported by robust evidence → Use with caution!
- Opioids + CPAP in decreasing respiratory distress prior in a patient that is NOT crashing
- PulmCrit- How to convert a VBG into an ABG
Dr Rhodes – Pediatric Asthma Exacerbation
- Asthma is super common in children… 3rd most common cause for pediatric hospitalization
- Questions:
- O2 sat objective
- PIS score (more subjective) or PRAM score for severity
- Bare minimum:
- B-2 agonist: Rac vs Levalbuterol (just more expensive, no benefit), neb = mdi (“at least as effective, 4-12 puffs”),
- “Rule of 5” for MDI
- 5 deep breaths, hold for 5 seconds
- Spacer
- In PEDS, 4 puffs = 5-10kg, 6 puffs = 10-20kg, 8 puffs >20kg
- In ADULTS (esp during COVID), can give 8x puffs of MDI (WITH SPACER) = equivalent medication 1x neb Tx
- “Rule of 5” for MDI
- B-2 agonist: Rac vs Levalbuterol (just more expensive, no benefit), neb = mdi (“at least as effective, 4-12 puffs”),
- Nebulizer
- Ipratropium
- 3 dosages
- Ipratropium bromide added to asthma treatment in the pediatric emergency department
- Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children
- No benefit after tres
- NNT 1:16 to avoid hospitalization
- Steroids
- Within 1 hour; NNT 1:8 to prevent admission
- IV vs oral? Same hospital admission rates
- “Dex is Best” -Geoff
- “Always consider your patient population – there may not be much of a difference but consider what you are asking of your patients… once a day for 5-7 days, vs once (with dex) and maybe one more additional dose at 72 hours” -Dr. Shah
- Magnesium
- Relax bronchial smooth muscle
- NNT 1:4 to avoid admission
- Dosing: 25-75 mg/kg; max 2g
- Adverse effect = hypotension (give IVF bolus)
- Rizzo: “asthma exacerbations have been related to magnesium deficiency.”
- Oral magnesium supplementation in asthmatic children: a double-blind randomized placebo-controlled trial/
- High-dose mag
- Dose: 50mg/kg/hr/4 hr
- “Conclusions: The early utilization of high-dose prolonged magnesium sulfate infusion (50 mg/kg/hr/4 hr), for non-infectious mediated asthma, expedites discharges from the emergency department with significant reduction in healthcare cost.”
- Heliox
- Can only use when FiO2 < 40%
- Ketamine
- Nebulized ketamine? YES!
- NIPPV / HFNC
- HFNC better better supported by evidence
- BiPAP may be difficult to get kids to wear
- Intubation
- Large tube
- High I:E ratio
- Chest xray?
- Not needed if mild
- If coughing for a few days prior? Consider it
- If admitting? Consider letting upstairs get it themselves (Do NOT be pressured to order beyond what you deem is necessary – YOU have evaluated the patient, not the floor team)
Serife – herbal supplements
- Valerian root
- St John Wort
- s/e: induce CYP-450; cyclophosphamide, warfarin, digoxin, oral contraceptives, theophylline, amitryptilline
- Ginkgo
- s/e: increase bleeding risk