Residency news and updates:
- None this week
We will be watching the first quarter of the 2021 EMRAP Cardiology Conference.
Lectures:
8a: Updates on ACS management / Managing Cardiogenic Shock / BREAK
9a: Hypertensive Emergencies / Chest Pain in Pregnancy / BREAK
10a: ECG Bootcamp #1 / Echo 101 / BREAK
11a: LVADs / Managing Acute Pulm Edema
Updates on ACS management
- Certain NSTEMI’s need reperfusion
- Immediate invasive (<2h) –
- refractory angina, recurrent angina, sustained VT/VF, hemodynamically unstable
- European guidelines: heart failure 2/2 to NSTEMI, or aVR STE w/ diffuse depressions
- Early invasive (2-24h):
- dynamic ECG (new STD), rising troponin
- Delayed invasive (24-72h):
- DM, CKD, EF < 40%, CABG/PCI w/i 6 month, or post-MI pain
- Meta-analysis khan;
- 25% of NSTEMI have OMI – need reperfusion
- OMI vs NOMI
- Meyers J emerg Med:
- 38% had occlusive disease w/o STE on ECG
- STE sensitivity not good in occlusive disease
- Meyers IJC Heart and Vasc 2021 Domo Arigato
- 41% sensitivity of diagnosing STEMI

- 90% had >2 findings, 4% had 0 of these findings
- DIFOCCULT trial – ⅓ of NSTEMI’s could be identified as OMI on ECG (NSTEMI A group)

- OMI-NOMI: Time for a Paradigm Shift
- Bottom line: Consider patient presentation, risk factors, ECG, subtle findings, biomarkers
- DAPT in NSTE-ACS:
- Increased bleeding risk, no increased benefit
- Do in discussion w cardiologist
- ISAR REACT 5: Ticagrelor (assumer better due to PLATO studies)
- Ticagrelor or Prasugrel in Patients with Acute Coronary Syndromes
- Prasugrel – lower MI; no difference in bleeding rates
- Europeans ahead again… use prasugrel
Managing Cardiogenic Shock by haney.mallemat@gmail.com @criticalcarenow
- Takotsubo cardiomyopathy – stress induced, can cause cardiogenic shock
- Compensated vs decompensated (with stressor, edema) vs cardiogenic shock (decreased perfusion to peripheral tissues)
- SCAPE
- more decompensated; hypertensive – not what this lecture is about

- Step1: Identify pt is in cardiogenic shock
- Vital signs, Mental status, Cap refill
- COLD extremities
- Hypotension
- Narrowing pulse pressure = sbp-dbp
- Step 2: Identify and confirm: Ultrasound
- RUSH exam, HIMAP mnemonic
- Step 3: Consult Early
- Step 4: Resuscitate
- Small boluses (250c)
- defend the MAP –increase coronary perfusion
- start with vasopressors first (NE) – don’t go above 10 mcg Levo, [then step 5: add inotropy – dobutamine (good beta)]
- Step 5: SUPERCHARGE Cardiac Output (add ionotropy)
- Dobutamine: good beta, can cause hypotension
- Epinephrine: good alpha and beta
- Milrinone: long half-life, can cause hypotension, stuck for 4-6 hours, worse if renal insufficiency
- Step 6: Check your work
- Monitor: central line, cvp, new labs (lactate), urine output
- Intubate?
- High risk for acidosis, hypotension, arrest
- Step 7: CABG, CAth lab?, thrombolysis (not primary unless transport…)
- Mechanical support –
- goals of care (temporary eg myocarditis, wait til PCI/transplant – not curative step)
- IABP: diastole balloon inflates, systole deflates for suction forward flow…
- Impella: sits in Left ventricle, pulls blood out of LV into aorta, impella vs IABP no difference…
- VA ECMO – cath retroperfuses heart, can actually do in the ED… maybe in the future
Hypertensive Emergencies by Jess Mason, MD
- Core Pendium chapter
- Hypertensive emergencies = severe elevations in BP (≥180/120 mm Hg) complicated by acute end-organ dysfunction.
- Lower bp by 20-25% in 1 hour – SBP
- End organ dysfunction aka “emergencies”
- Neuro emergencies: PRES/RPLS, HTN encephalopathy
- Cardiac: ACS
- Pulm: SCAPE
- Renal: ARF
- Other: retinal hemorrhages, eclampsia/pre-eclampsia, pheochromocytoma
- Neuro HTN emergency: nicardipine – quick on and titratable
- Aortic dissection: reduce HR and bp, esmolol, quick on and off, can add nicardipine for bp (labetalol has 7x more beta blockade than alpha therefore not great for bp)
- SBP <120 HR <60
- ACS and pulmonary edema: NG
- Renal: fenoldopam – less renal injury (or nicardipine in a normal world…)
Chest Pain in Pregnancy by Britt Guest, DO
- Increase in maternal death:
- due to death from cardiomyopathy, CVA, cardiovascular “catastrophes”
- Risk factors:
- Race/ethnicity: African americans >3.4x risk of dying
- Age >40y/o >30x higher than 20 y/o female
- HTN: increases risk of MI 13x; Heart failure 8x
- Pt presentations: chest pain, sob, palpitations
- Uncomfortable causes:
- acid reflux, rib pain, increased RR, increased minute ventilation, Inc HR (15-20%)
- Pregnant = natural stress test:
- inc O2 demand, increased minute ventilation, increased blood volume (inc O2 carrying capacity), inc CO
- Total Blood Volume up by 50%, CO up by 30-50%
- IVC compression – dec venous return, Aorta compression – inc afterload
- Dangerous causes
- MI: 3x higher risk, majority have it postpartum period, cardiac muscle takes a year to return to normal
- Causes: SCAD (43%), coronary atherosclerosis, thrombus in normal artery, coronary spasm
- SCAD vs atherosclerosis – dx made in cath lab
- Atherosclerosis: PCI preferred over thrombolysis, ASA + Hep
- SCAD: conservative management – stent may worsen dissection, heparin could make problem worse
- PE: clinical prediction rules not validated in pregnant pt’s, D-dimer increased normally in pregnancy, definitive dx requires imaging
- Pregnancy-Adapted YEARS Algorithm for Diagnosis of Suspected Pulmonary Embolism
- Risk for radiation associated fetal abnormalities = 50 mGy
- VQ scan = 0.32-0.74 mGy
- CTPA = 0.03-0.66 mGy
- Imaging should not be delayed if you suspect PE
- Tx: heparin (does not cross placenta)
- 1st line: LMWH (lower risk of bleeding)
- 2nd line: unfractionated heparin (use if renal dysfunction)
- AVOID DOACS OR WARFARIN
- Postpartum cardiomyopathy: “rare” 1/1000 cases
- Risk factors: increased age, multifetal pregnancies, gestational HTN
- Workup:
- Bnp increase in normal pregnancy–not most reliable
- ECG
- ECHO!
- Diagnosing PPCM:
- HF in late pregnancy or up to 5 months postpartum
- No other cause for HF
- LVEF <45%
- Diagnosing PPCM:
- Acute HF: loop, CPAP/BIPAP, NG
- Long-term: AC (hep), BB, Dig
- Prognosis: linked to LVEF
- EF< 30%: 5-10% rate of death or cardiac transplant 1 year postpartum
- Take home points:
- Cp, sob, palpitations-normal changes OR pathologic?
- Risk of cmy, pe, ami is higher in 3rd trimester and postpartum
- If you need imaging study-get it
- Ami think SCAD–avoid heparin and thrombolytics
- Treatment of pregnant patient is similar to non pregnant patients
ECG Bootcamp #1 by Amal Mattu, MD
- MI in LBBB
- ECG:
- STE in contiguous, posterior STEMI, LBBB with sgarbossa, pacemaker with sgarbossa, post-arrest ACS (no longer new LBBB since 2013)
- Rule of appropriate discordance:
- QRS up, little STD (ST should never be in the same direction); OR QRS down, little STE
- Sgarbossa
- A – concordant STE > 1 mm any lead – very specific, doesn’t need to be contiguous
- B – concordant STD > 1 V1, V2, or V3 – very specific, doesn’t need to be contiguous
- (V1, V2, V3 where the QRS normally points down)
- C – discordant STE > 5 mm (not in modified; less specific)
- (When the QRS points down, you normally see a little bit of STE)
- Revised/modified Sgarbossa
- A and B are the same.
- Modified C: STD:S-wave > 25% – really accurate
- Ratio of STD:S wave size more useful than 5 mm
- Takehome: revised sgarbossa…
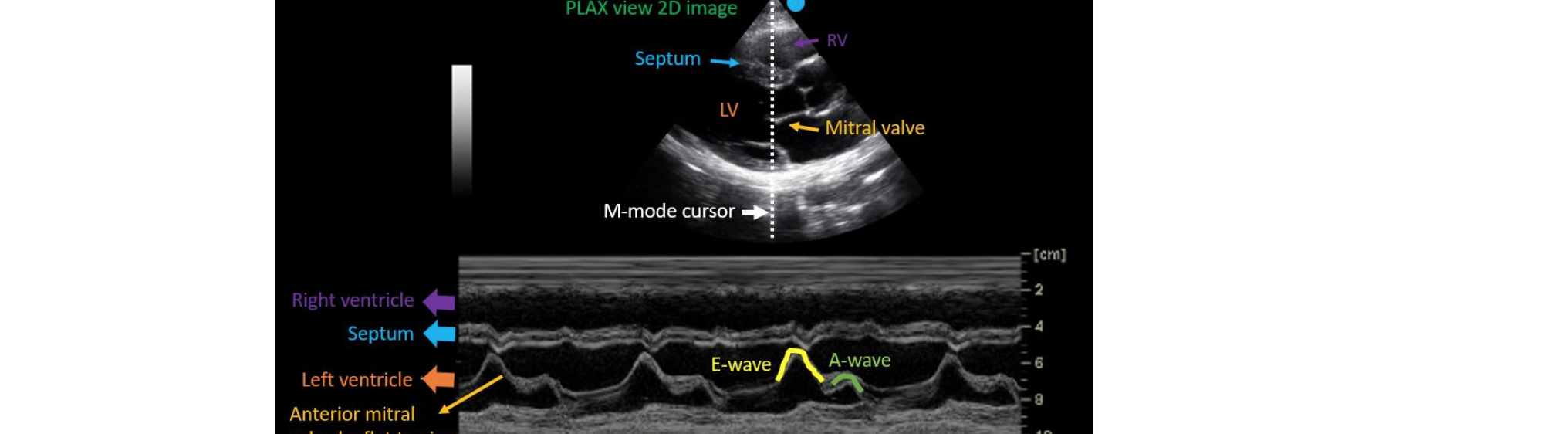
Echo 101 by Amir Tabibnia, DO
- Cardiac US indications: effusion/tamponade, undifferentiated hypotension, dyspnea, cardiac arrest, TVP, syncope, blunt trauma, acute chest pain
- Phased array probe w cardiac preset.
- Parasternal long: cardiac convention (marker to R shoulder), ED (L hip)
- Parasternal short: cardiac convention (L shoulder)
- 4 chamber probe L
- Subxiphoid : probe left
- IVF: probe inferior
- PSL

- Something about a diamond ¯\_(ツ)_/¯ – rule of thirds; L atrium, outflow tract, and RV should all be equivalent size
- LV systolic function: assess muscle thinning or thickening
- EPSS – 0.7; LVEF = 75.5 – (2.5 x EPSS)
- Fractional shortening – endocardium of free wall and interventricular septum should come in 25-40% is normal
- PSS – 3 views; high parasternal, mid parasternal (fish mouth); low parasternal (money shot, papillary muscles)
- Good for wall motion abnormalities
- WMA: compare to ECG, limited assessment of WMA in LVH
- SALPI mnemonic

- A4C
- Good for takotsubo
- Can assess WMA and EPSS

- SX
- Great for pericardial effusions (dynamic view, tilt to look for pericardial effusions)

LVADs– ran out of time
Managing Acute Pulm Edema
- Heart Failure | CorePendium
- Not all pulmonary edema is cardiogenic…
- Diastolic heart failure (preserved EF): heart doesn’t relax, can’t fill properly
- Systolic (reduced EF)
- R sided HF → fluid backs up into body
- APE:
- Sympathetic overdrive
- Fluid in lung → resp distress → terrifying → sympathetic response → peripheral vasoconstriction (inc afterload) → worsens renal perfusion → RAAS activation → sodium retention and more vasoconstriction → redistribution of blood → inc preload
- BIPAP vs CPAP
- fairly equivocal- Core compendium.
- start CPAP at 10 cm H2O or BiPAP at 10/5 cm H2O and adjusting up as the patient tolerates and with clinical response.
- FiO2 @100%
- US: B lines, anterior lung fields, more than 3 between 2 ribs
- BLUE protocol: 97% sensitive, 95% specific
- 1-2 B-lines just means inc pulmonary density, means nothing, huge differential
- CXR
- Can suggest volume overload
- NG
- Lower doses: decrease preload (<100 mcg/min(
- Afterload reduction at 100-250 mcg/min
- Start IV infusion at 400 mcg/min for 2-5 min and titrate (she starts high and titrates down)
- SL 400 mcg = 80 mcg/min IV bioavailability-wise
- Bolus dosing NG prevents ICU admission; can go up to 1-2 mg
- Beware if preload dependent eg pericardial tamponade
- Ask about viagra…
- ACE inhibitor for afterload reduction
- Beware if renal impairment
- Not 1st line, after initial resuscitation
- Captopril, enalaprilat
- Morphine: Increased 30d mortality
- Except hospice/palliative
- Diuretics
- Not initially
- Good if total body volume overload (not just lungs)
- Effective if poor renal perfusion
- APE + Hypotensive: High mortality, cardiogenic shock
- Fluid challenge (250-500 cc aliquots)
- Pressors – NE