- 7a: Dr Shee – LVADs in the ED
- 8a: Resident Lectures: Geoff – Bradyarrhythmias / BJ – Trauma
- 9a: Dr Rizzo – How To Call A Consultant–postponed for another day / Dr Rizzo – SAH podcast (last week’s)
- 10a: Break / Mallory – Addiction Lecture (Methadone and other opioids)—postponed for another day
- 11a: Dr Jeong – Core Concept Lecture –postponed for another day
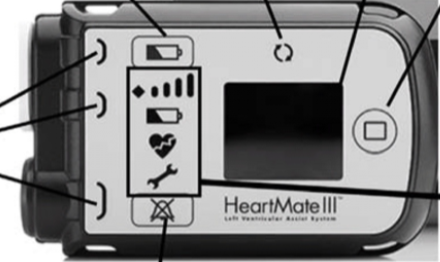
- Dr Shee – LVADs in the ED
- LVAD = continuous flow, no pulse, DO have a MAP, use manual cuff or US
- How to get MAP with US: find radial artery, inflate cuff until no flow, when flow starts as you deflate.. That’s your MAP (70-90 NORM; 80 goal)
- Sick? Consider a-line
- Pulse ox–needs a pulse, LVAD pts don’t have a pulse
- Echo: LV will always be dilated; need to look at RV to see if it can supply the LV with blood OR if there is a giant PE
- LVAD is bridge to heart transplant, or temporary for condition you probably will recover from (Takotsubo)
- Volume status? Taking diuretics,diarrhea, etc
- Pulse index?
- Anticoagulated, goal INR: 2-3
- https://rebelem.com/left-ventricular-assist-device/
- CPR should be performed only if absolutely necessary, but remember this might lead to damage of the VAD itself. There was a small retrospective case series of 8 patients with VADs who received CPR during cardiac arrest, which showed no dislodgement or damage to the VADs, and 4 of the 8 patients surviving with neurologically good outcomes, but larger trials are needed before making this the standard practice. [5]
- Not perfusing: End tidal <20, MAP <50? —> START CPR
- Battery alarm going off–you have five battery minutes
- PI number >3
- Pump power:
- LVAD = continuous flow, no pulse, DO have a MAP, use manual cuff or US
- EMCRIT
- https://emcrit.org/emcrit/left-ventricular-assist-devices-lvads-2/
- Poor Perfusion
- When in doubt, consider a fluid bolus. VADS love volume. If you need to improve hemodynamics with a working LVAD, consider preload augmentation and possibly afterload reduction (if MAP is high).
- Consider inotropes–if you think it is right heart failure, give dobutamine. If you think the patient is septic and has markedly reduced afterload, consider norepinephrine.
- Low flow: consider sepsis
- HIGH FUNGAL INFECTION RATES DUE TO LINE PLACEMENT–get fungal cultures, blood cultures
- ECG: a lot will have AICD as well–with BB pattern
- Vtach can be either ventricle and they don’t know/feel it
- STEMI-LVAD is doing all work, so
- Bleeding-
- GI bleeding
- Do not reverse anticoagulants–continue giving them blood and they can get scoped.
- HEMORRHAGIC STROKE:
- High chances as on blood thinners and high MAP
- Embolic stroke
- Can NOT GIVE TPA—contraindicated on blood thinners, get them to endovascular thrombectomy
- GI bleeding
- Infected LVAD?
- CT surgery: likely want pan scan chest/abd/pelvis
TINTANELLI’S ONLY PAGE ON LVAD ^^- Geoff – Bradyarrhythmias
- Case: hypotension, bradycardic ℅ CP
- What should you first do? IV, O2, monitor, pads
- Start: atropine, dirty epi, IVF
- Case: AMS s/p rollover MVC—BP: 175/120, HR 32, O2-92%
- Cushings: hypertensive, bradycardic, decreased RR
- Cerebral t waves
- BRASH syndrome-Bradycardia, Renal disease,
- Hyperkalemia tx: 1g CaCl, 3g CaGluc; insulin/dextrose, albuterol–or epi
- Epi drip, IVF
- With multi comorbidities/polypharmacy: Consider Beta blocker/calcium channel blocker/digoxin toxicity.
- BB/CCB: tx w high dose insulin, intralipid–other treatments as well
- Digoxin: tx with magnesium, digifab –other treatments as well
- Hyperkalemia tx: 1g CaCl, 3g CaGluc; insulin/dextrose, albuterol–or epi
- Step 1: IV, O2, monitor, pads-defib/pacing; crash cart
- Step 2: Stable vs unstable patient
- MEDICATIONS are faster than procedures (usually)
- Step 3: Wide or narrow complex on ECG/Monitor
- Step 4: P waves? Present or not
- Step 5: POSSIBLE CAUSES of bradycardia: “HE DIE”
- Hypothermia
- Endocrine
- Drugs
- Ischemia
- Electrolytes
- Universal protocol
- Atropine: 0.5mg q IV q5min x3-6 max: 0.04mg/kg ~3mg
- Antimuscarinic → decreases vagal stimulation
- ACLS 2020 update: atropine dosing increased from 0.5mg to 1mg
- Epinephrine:
- ACLS dosing = 2-10mcg/min
- Dirty epi drip vs push dose.
- Atropine: 0.5mg q IV q5min x3-6 max: 0.04mg/kg ~3mg
- Dopamine:
- Increases HR, contractility, CO
- ACLS dosing: 2-20mch/kg/min
- Isoproterenol
- Non-selective beta agonist that can “get a heart rate out of a rock”
- Dosing: start at 5cg/min (2-10mcg/min)
- Pacing:
- Transcutaneous pacing
- Transvenous pacing
- Case: hypotension, bradycardic ℅ CP
- BJ – Trauma
- ABCDE
- Airway –protecting vs intact
- Obstruction? ALOC? Trauma to face?
- Intubate, -C- collar
- Breathing –ventilation, auscultate
- Jvd, tracheal position…
- Chest decompression: tension/massive/open PTX
- Circulation–
- Hypotension == blood loss
- Internal bleeding: can give up to 1.5 L; >1.5L increases odds ratio of death
- Hypotension and BRADYCARDIA == neurogenic shock
- Check: Central and peripheral pulses
- Hypotension == blood loss
- Disability:
- Neurologic evaluation
- GCS–higher level = better outcome
- PREVENT FURTHER BRAIN INJURY by maintaining oxygenation and perfusion
- Exposure/Environmental:
- Fully undress the patient. Cut them off
- Environmental: hypothermia/ also decontamination
- Roll patient, feel spine for step-offs/tenderness; place xray plates
- Look for level of injury
- Look in between legs, do rectal
- Airway –protecting vs intact
- What to say in ressuss room:
- A: “Patient protecting airway, no visible obstruction or deformities”
- “Airway intact”
- B: “Breath sounds auscultated in bilateral lungs w appreciable chest rise that is equal on both sides”:
- C: “ Central pulses intact-distal pulses intact.”
- D: “ Patient a&Ox3, opening eyes spontaneously, responding appropriately to commands, pupils equally round and reactive to light.”
- E: “ NO signs of additional trauma on back, no midline TTP of C/T/L spine, no appreciable deformity or stepoff, no visible trauma to perineum, rectal tone intact.”
- PT CONDITION HAS CHANGED:
- Restart the PRIMARY survey.
- A: “Patient protecting airway, no visible obstruction or deformities”
- ABCDE
- Dr Rizzo – SAH podcast (last week’s)
- Link: https://coreem.net/podcast/episode-181-0-subarachnoid-hemorrhage/
- Sudden onset, worse at onset
- Don’t ask “are you having the worst headache of your life?” — it’s a priming question
- Non-con CT, 125 slides = high res CT
- Inclusion criteria of studies, pay attention, inclusion criteria for SAH rule new HA = headache <14 days — apply decision rules to the right population.
- https://www.mdcalc.com/ottawa-subarachnoid-hemorrhage-sah-rule-headache-evaluation#use-cases
- Live on NY (organ transplant): 1-800-GIFT-4-NY (443-8469)
- Speaker: Rene Mascoll:
- 917-701-9194
- rmascoll@liveonny.org
- 145 people added to waitlists per day just in our area
- 1 donor can save 8-9 lives (liver can be two donations)
- WHEN TO CALL:
- Within 1 hour for any of the following:
- Potential organ donors:
- Loss of 2 or more brain stem reflexes
- GCS <5
- Prior to any end of life discussions with patients family
- Potential tusse donors: have 24 hrs for procurement–keep eyelids closed and head slightly elevated to protect eye/cornea donation
- all deaths
- Cardio-respiratory death: pt expired in ressuss
- Potential organ donors:
- No call is too early: refer all vent-dependent patients at first indication of a non-survivable neurologic or anoxic injury or illness.
- Within 1 hour for any of the following:
- **The hospital cannot legally terminally extubate a patient WITHOUT live on new york evaluation.
- LONY is HIPPAA privileged—can give HIPPA information on phone or in person.
- Covid positive donors can give organs to covid negative.
- Per LONY, physicians are NOT supposed to talk about organ donation with patients.
- Speaker: Rene Mascoll:
- DR. KINDSCHUH:
- JCO is HERE
- First annual community outreach: August 11 9am-12noon—Dr. Kindschuh beach house in Breezy point
- Volunteers needed
- Planning on some health fair education/show and tell
- Ideas for education:
- Pediatrics: germs/viruses
- Elderly patients;
- How to identify strokes
- HTN/BG screening
- Injury prevention in home
- PR rep: Bridget