The “Dislodged” PEG Tube
This is a CLASSIC Coney patient. 83yr old nursing home patient arrives with chief complaint of “dislodge peg tube” or “peg tube needs replacement”, completely contracted and luckily the nursing home staff was nice enough to send the chewed up old tube in a chuck with the patient.
–>What do you do next? What if this tube has been out for an extended period of time? What if the tube is still in the patient but they are requesting a change?
Step 1: Determine the time frame the tube was placed AND how long the tube has been dislodged
Any tube placed within 2-4 weeks must be replaced by the team that originally placed the tube (GI, IR, Surgery)
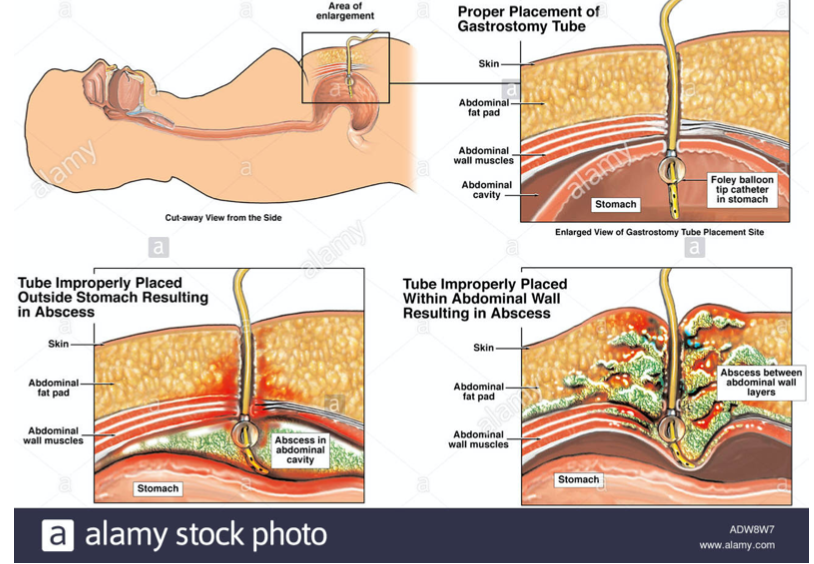
the percutaneous track has not had the chance to mature, so ED replacement can possibly lead to an intra- pertoneal tube
If a mature tube (placed >4 weeks ago) as been dislodged less than 24 hours, it is probable safe to replace in the ED. However, keep in mind that even a mature track can close within 8 hours so be prompt in your peg tube replacement
Step 2: Determine the size and type of tube
Most tubes are between 16F-24F, you can look for the label for tube size at the feeding/balloon ports.
If the patient is coming from a nursing home, it is sometimes listed in their papers (if the tube is unavailable).
Remember: G (gastrostomy) tubes are replaceable in the ED, G-J (gastro-jejunostomy) tubes and J tubes typically needs to be replaced by GI/Surgery/IR (we do not carry G-J or J tubes in our ED)
Step 3: Prepare the supplies and the patient
Gather the equivalent size of the G Tube, gloves, lube, 10cc syringe with saline, temperature probe cover, omnipaque, 30-60 cc syringe
Place the patient supine, if contracted ask for a helping hand as you may have a difficult time fighting limbs and contracted abdominal muscles
Inspect the abdomen for any signs of infection or perforation
Step 4: Placing the tube
Using the temperature probe cover, you can see if the track for the PEG tube is viable (be sure to hold onto the end tightly!)
After checking for viability of the track, next test the balloon of the new gastrostomy tube and place lube at the end that will be entering the track
Apply constant pressure while feeding the tube into the track. If you encounter tense abdominal muscles, press on the muscles with constant pressure until you feel give and can advance the tube
Inflate the balloon with indicated amount of saline (usually listed on balloon port or package insert) and pull back on the tubing
Note: If we do not have the appropriate size G tube, use a foley to keep the track patent
Step 5: Checking placement of the tube
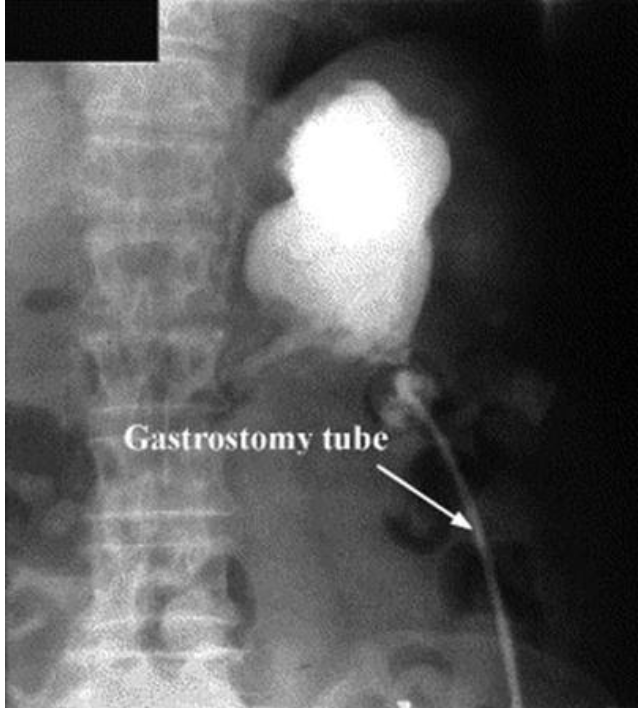
With x-ray at bedside, check placement by inserting up to 30ccs of omnipaque into the feeding port You can check for gastric contents by pulling back on the feeding port… looking something like this:

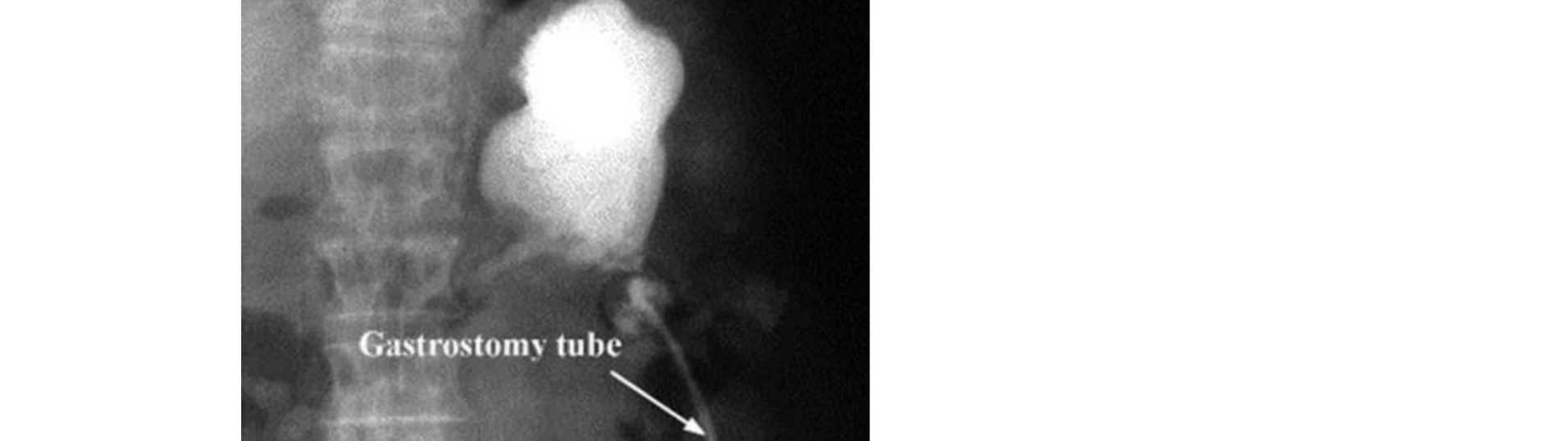
Confirmed placement on xray should look something like this:
Where a misplaced tube would look more like this:

Step 6: Dressing and discharge
Depending on the tube, the outer bumper can be adjusted to just about a 1/2 inch above the skin
Gastroenterology literature and our own GI fellows note to not place 4x4s between outer bumper and skin, some recommending to not tape down the PEG tube at the entry site
If the patient is the combative type that had pulled out their own tube, taping the tube in a way to prevent dislodgement but avoid tissue breakdown at the tube’s entry to the stomach
If you were unable to place a tube and are currently using the foley as a placeholder, contact the appropriate team for proper tube palcement
Tips and Tricks
Is the patient in the ED due to a clogged G-tube?
If it is confirmed that the tube is in the appropriate place, try to pull back on the clogged particles with a syringe Introducing warm water in back and forth pumping movement with the syringe can help break up some particles further
You can use a guidewire to clear portions that are above the subcutaneous parts of the tube
Although not back by evidence, I have seen the coca-cola trick work in person with GI, so might not hurt to give it
a try!
Is the gastric tube leaking?
Any leakage of gastric contents on the subcutaneous or into the peritoneal cavity can cause major problems and infection for the patient
Suspend feeding and discuss the case with the team that placed the tube (GI/Surgery/IR)
It says it’s a G tube but I can’t remove it/it feels like it’s stuck!
You may have come across a tube with a mushroom bumper, which would need to be addressed by the team that placed the tube. Mushroom bumpers look like this internally:
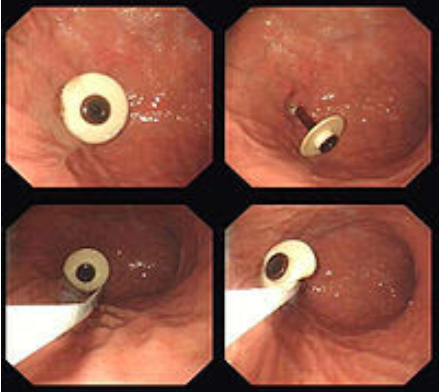
If tube tube is not mobile within the stoma, you may have a patient with buried bummer syndrome (usually seen in PEG tubes placed within a year)
This occurs when the bolster inside the stomach produces ischemic necrosis of the gastric mucosa and migrates into the gastric wall/subcutaneous tissue
This is an emergency as further tampering can lead to pain, possible perforation, so please place a consult to Surgery (+/- ct abd) with antibiotic coverage
Happy Tube Feeding!!