Urinary Tract Infection
The Case: 60-something year old male presents to the ED with signs of urinary frequency and feelings of incomplete voiding. When you see the UA results there are moderate nitrites, moderate leukocyte esterases but NO urine bacteria. Your attending turns to you and says “Why did you order rocephin for sterile pyuria, there are no bacteria”, and you turn to your attending to say “because I should have finished this Sunday scary weeks ago. i loathe weird UAs”
The UTI Breakdown
Upper and Lower Urinary Tract
Upper = Kidneys and Ureter (Pyelonephritis) Lower = confined to the bladder (Cystitis)
Complicated vs Uncomplicated
Complicated = patients with increased rate of treatment failure, ALL pregnant women, ALL old men (really men in general), Upper UTIs, moderate/severe diabetes, immunocompromised, pt with kidney stones, individuals with anatomic abnormalities, indwelling catheters or ureter stents
Clinically: febrile, weakness, AMS, abdominal pain
Bacteria: VRE, pseudomonas, ESBL E.Coli Uncomplicated = acute cystitis, nontoxic pyelonephritis
Clinically: dysuria, hematuria, urgency, frequency, suprapubic pain
Bacteria: E. Coli (75-90%), staph saprophyticus, klebsiellla, proteus, enterococci
Relapse vs Reinfection
Relapse = recurrence of UTI symptoms within a month –> same organism –> treatment failure Reinfection = symptoms in one-six months after treatment –> different organism
*if a patient presents more than 3 times in a year consider undiagnosed diabetes, renal calculi, urinary tract tumor*
Diagnosis
*Remember UTI and pyelonephritis are clinical diagnoses, where a patient’s self diagnosis has a likelihood ratio of 4.0 (90% accuracy–as accurate as a dipstick)
*In young females, likelihood ratio increases to 24.6 with symptoms of dysuria and frequency in the absence of vaginal discharge or irritation
Review: -don’t let urine specimens sit for longer than 2 hours
-UA testing in most cases is not required (more for primary care)
-Although midstream is gold standard, no real difference between collection w/o cleaning (great because those
wipes are a rarity in the ED)
UA: WBC count = >5 with symptoms is diagnostic
WBC count 1-2 with bacteriuria = significant in men –> consider STI
High WBCs w/o bacteria = consider STI, appendicitis
Leukocyte Esterase = high specificity, low sensitivity
Nitrite = very high specificity, does not detect enterococcus, pseudomonas, acinetobacter
To urine culture or not urine culture, that is the question
- Suspected complicated UTI
- Relapse/reinfection
- Suspected Upper UTI
- Children
- Pregnant females
- Males
- Recent instrumentation-Cultures provide little to no additional information for the uncomplicated infection-23 = # needed to test in order to prevent follow up consultation –> cost absolutely outweighs benefitSo when is the culture positive??-traditionally = 10^5 CFU per ml
-those with + UTI symptoms usually only have 100-10^2 CFUs per mL
-all the reason we don’t use it for initiation of treatment and further why they should not be used in theuncomplicated UTI
Fun Fact: Organism in blood cultures match the urine cultures in 97% of the cases. Do them in your urosepsis patients only (CMS will hate me for this EBM)
Treatment
Side Note: STOP treating asymptomatic bacteriuria (in the non-pregnant individual or non-pre-OP individual or non-renal transplant individual)
-Just like pain is not an indication for oxygen ( 
for treatment.
–NOT associated with long-term development of sepsis, pyelonephritis, or renal failure
-2005 placebo controlled trials (IDSA guidelines) even showed that abx use doesn’t even prevent the rate of symptomatic UTI
Sweet Little Review Table
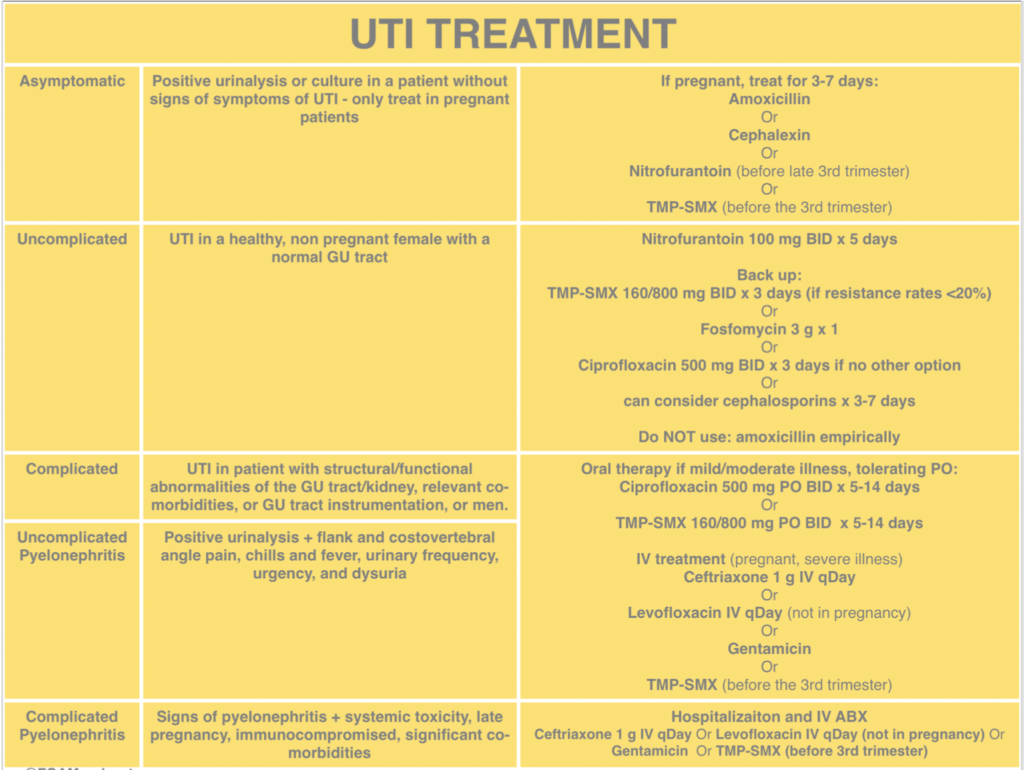
EM:Rap’s Nov 2018 Pharm Rounds
Nitrofurantoin is preferred in uncomplicated UTI and in older adults as long as their creatinine clearanceis >40ml/min
Fosfomycin is difficult for that average patient to obtain and less effective but is good for that one time dose in the ED (3g PO). Is effective against ESBL and VRE, and safe in pregnancy
The Uncomplicated UTI = abx for 3-5 days The Pyelonephritis = abx for 10-14 days
Dosages
*Fun fact* majority of cystitis is self resolving : two placebo studies (population: young healthy females) showed
cure rates of 55% and 70% when compared with abx use. 
Cystitis
Nitrofurantoin 100mg BID 5-7 days (90% cure rate-bacteriostatic at 7 days) TMP-SMX DS BID 3 days (95% cure rate)
Or just TMP 100mg BID 3 days
Cephalexin 250mg BID 3 days
Cipro 250mg BID 3 days (if you don’t care about your patients CNS, mental health or legs)
Pyelonephritis
Cipro 500mg BID 7days Levofloxacin 750mg BID 5 days
the quinolones are unfortunately still listed as 1st line so this is your exam answer my friends Cefpodoxime 200mg BID 10-14 days
TMP-SMX BID 14 days
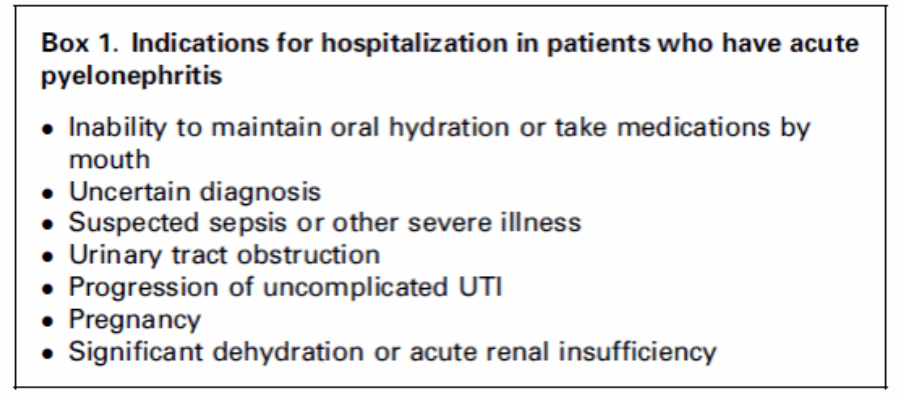
When to Admit that Pyelo
*Majority of pyelonephritis can be sent home with a 48 hour follow up
ED if they continue to have fevers or still feel ill
*Here are some guidelines for helping you decide if this individual needs to stay
Take Home Points
- UTI and pyelonephritis are clinical diagnoses
- Dysuria + Urinary Frequency – STI symptoms = UTI diagnosis even w/o a UA
- Get that UA in the immunocompromised, pregnant, previous abx use
- Think twice before you get a urine culture
- Stop treating asymptomatic bacteriuria in the average patient
- Stop getting imaging for clinical pyelonephritis
- The essential oils of UTI treatment: cranberry juice, direction of wiping, post-coital urination, and that one dose of IV abx before discharging from the ED (we’re giving them abx associated diarrhea for our own comfort)

