What do you really know about the Urine Analysis?
Daily Questions on Shift: This UA shows negative nitrites, negative leuks but TNTC bacteria. “WHAT?!” UA shows multiple epithelial cells. “okay this patient didn’t listen to my request for a clean catch”. (or my recent favorite) my inbox: urine culture shows “why the hell did i order a culture and now i’m the only one to respond to this!?!?”
Urine has been really pissing me off lately.

Things we might have forgotten about Urine:
-Bedside Analysis: Color, Transparency, Odor, Dipstick
Color: As much as knowing the color of the urine is a pimp favorite for some ICU attendings, looking at the urine at bedside can really help us broaden our differential.
Green: Propofol
Orange: Rifampicin, Warfarin
Red: Kidney Stones, Trauma, schistosomiasis
Red-Brown: rhabdo
Purple: infections with klebsiella pneumoniae, p. aeruginosa
Black: methemoglobinuria
Complete list with helpful pictures: https://lifeinthefastlane.com/investigations/urine-colour/ Transparency: We all know that reaction after the suspected urosepsis patient is finally catheterized and it looks
closer to substance from an I&D rather than urine
Cloudy: mucus/epithelial cells Milky: fat globules
Smoky: blood cells
Complete list: https://lifeinthefastlane.com/investigations/urine-transparency/ Odor: Pretty gross but pretty helpful (if anything maybe for board exams )
Sweet/Fruity: Ketoacidosis Musty: PKU
Ammonia: retention/infection
complete list: https://lifeinthefastlane.com/investigations/urine-odour/
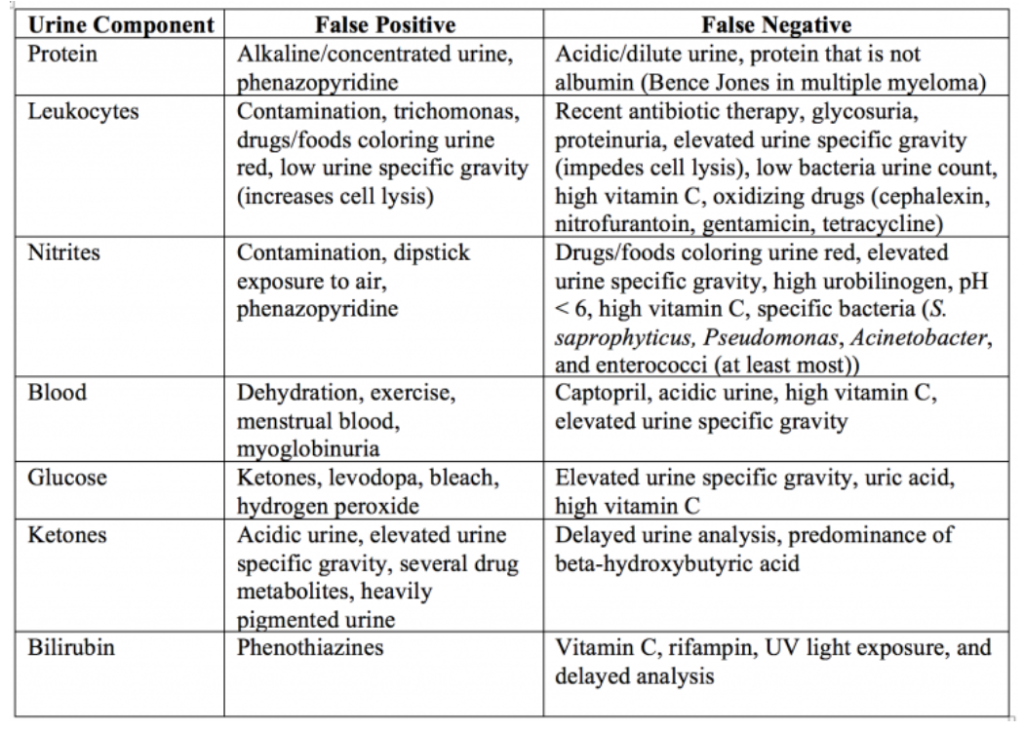
Dipstick: not really thought to improve diagnosis
-Looking at leukocyte esterase AND nitrites brings the sensitivity to 50% with specificity to close to 100% compared to looking at leukocyte esterase OR nitrites with a sensitivity of 75-94% and specificity of 82%
-If dipsticks are used alone there is a rate of over treating up to 47% with missing about 13% of UTIs
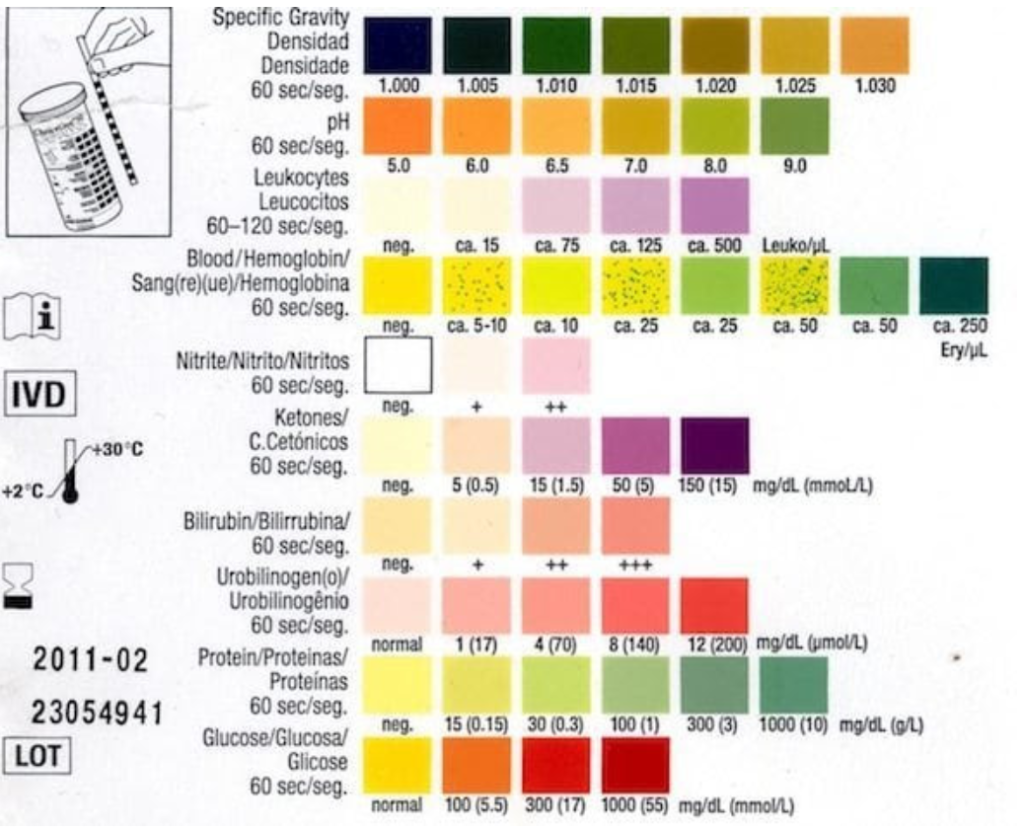
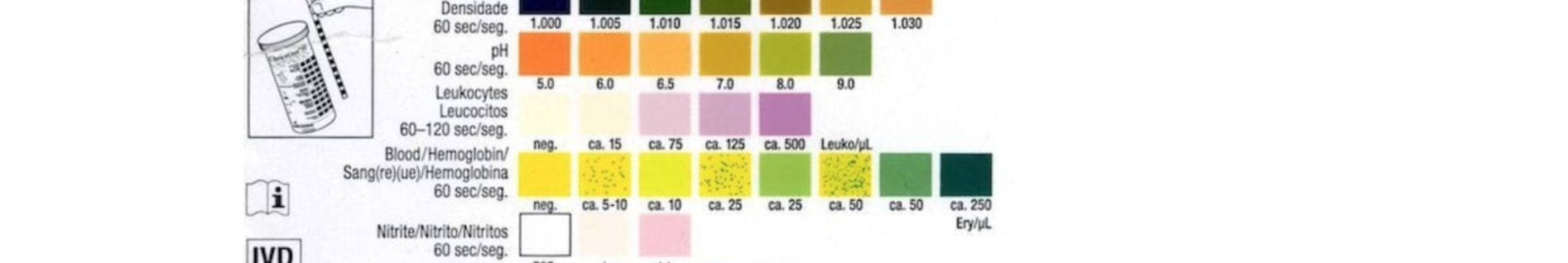
Specific Gravity
-Measurement of the ability of the kidney to concentrate/dilute the urine
-Assuming renal function is normal, specific gravity is normal btwn 1.002-1.035 (remember that water has specific gravity of 1.000)
–Decreased (<1.005): can indicate excessive hydration vs renal injury
– think nephrogenic diabetes insipidus, acute glomerulonephritis, ATN, pyelo
–Increased (>1.035): large volume of dissolved solutes
– Dehydration, SIADH, adrenal insufficiency, liver failure, nephrotic syndrome
–Fixed (1.010): more for the people upstairs or maybe our frequent fliers that we might be able to use as an admission argument point for chronic renal failure
pH (4.5-8.0)
–High urine pH (Alkalized): may suggest systemic alkalosis, renal tubular acidosis, old sample (be sure the urine is sent w.in the first hour of obtaining the sample). helpful in TCA overdose and rhabdo
–Low urine pH (Acidic): DM, starvation, PKU, malabsorption Protein
-Elevation could include:
Renal: Increased renal tubular secretion,increased glomerular filtration (glomerular disease), nephrotic syndrome, pyelonephritis, glomerulonephritis, malignant hypertension
CVS: Benign HT, CCF, SBE
Functional proteinuria (albuminuria): fever, cold exposure, stress, pregnancy, eclampsia, CHF, shock, severe exercise
Other: Orthostatic proteinuria, electric current injury, hypokalemia, Cushing’s syndrome
Drugs: Aminoglycosides, gold, amphotericin, NSAID, sulfonamides, penicillins
Nitrites and Leukocyte Esterase
-Nitrites: 90% specific/50% sensitive in detecting gram negative bacteria, positive test suggest bacteria but negative tests does not rule out infection
–Leukocyte Esterase: located in WBCs, appear when the lyse. 70% sensitive/50% specifc. False negatives related to glycosuria, proteinuria, high specific gravity
Blood, Glucose, Ketones
–Blood: related to hematuria, hemoglobinuria, myoglobinuria but does not tell us where the blood comes from -Glucose: reduced renal threshold or elevated blood glucose (diabetics and pregnant women)
–Ketones: starvation, alcoholism, DKA, eclampsia, hyperthyroidism. Overdose of insulin, isoniazid, isopropyl alcohol
Bilirubin and Urobilinogen
-Bilirubin: liver disease as bilirubin is not present in healthy urine. It is the failure of conjugated bilirubin to reach the intestines (think: biliary obstruction). Think hepatitis, cirrhosis, biliary tract obstruction, pancreatic obstructive jaundice. –Urobilinogen: although present in low concentrations when increased can indicate liver damage, hemolytic disease, and severe disease such as malaria, mono, hepatitis.
Guide to the Microscopic
best accuracy if <5 epithelial cells/HPF (15-20 cells indicated contamination)
>3 WBCs/HPF as lab cutoff (leading to the 44% overtreatment)
RBCs: glomerular (proteinuria, RBC casts, dysmorphic RBCs) vs nonglomerular (no RBC casts or dysmorphic RBCs)
And the ever boring but maybe it will help someone on some exam, somewhere….
Casts: Red cell casts – glomerulonephritis or vasculitis
White cell casts – tubulointerstitial nephritis, acute pyelonephritis, renal tuberculosis, vaginal infection Muddy-brown granular casts -acute tubular necrosis
Waxy and broad casts – advanced renal failure
Fatty casts – nephrotic syndrome
Crystals: May be totally normal
Calcium oxalate crystals – ethylene glycol ingestion
Uric acid crystals – tumor lysis syndrome, gout
Cystine crystals – cystinuria
Magnesium ammonium phosphate and triple phosphate crystals – UTI caused by Proteus, Klebsiella
Stay tuned next week for discussions of UTIs
References:
- https://lifeinthefastlane.com/investigations/urinalysis/ https://first10em.com/uti/
- https://wikem.org/wiki/Urine_analysis
- https://emergencymedicinecases.com/uti-myths-misconceptions/